一、冠状动脉痉挛CAS
◆ 1845 年,Latham 提出冠状动脉痉挛( coronary artery spasm,CAS)可导致心绞痛。
◆ 1959 年Prinzmetal 等首先观察到一组与劳力性心绞痛不同的心绞痛患者,常于静息状态下发作,伴有心电图ST 段抬高,命名为变异型心绞痛。此类患者不伴有心肌耗氧量的增加,是由于冠状动脉紧张度增加引起心肌供血不足所致。
二、冠状动脉痉挛综合征CASS
CAS 是一种病理生理状态,因发生痉挛的部位、严重程度以及有无侧支循环等差异而表现为不同的临床类型,包括:
(1)CAS 引起的典型变异型心绞痛
(2)非典型CAS 性心绞痛
(3)CAS诱发的急性心肌梗死(AMI)
(4)CAS诱发的猝死
(5)CAS诱发的各类心律失常
(6)CAS诱发的心力衰竭
(7)CAS诱发的无症状性心肌缺血
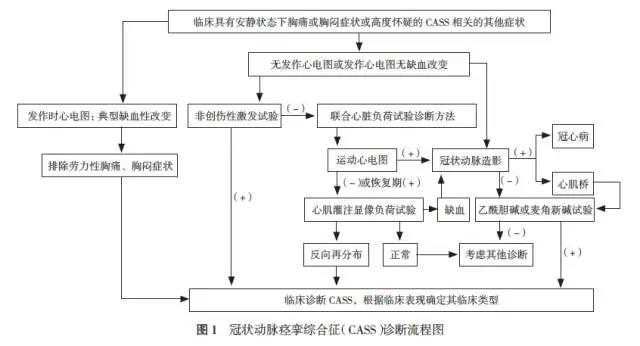
三、CASS的诊断
四、冠状动脉痉挛综合征的治疗
1、急性发作期的治疗原则:迅速缓解持续性CAS 状态
(1)硝酸酯类药物:首选硝酸甘油,舌下含服或喷雾剂口腔内喷雾。
(2)CCB:短效CCB,与硝酸酯类药物联用能提高疗效;推荐地尔硫草卓静滴或冠状动脉内注射。
(3)镇静镇痛药物:慎用吗啡。
(4)抗血小板药物:应尽早使用,可予阿司匹林300 mg 和氯吡格雷300~600 mg 负荷剂量,后续阿司匹林100 mg/d 和氯吡格雷75 mg/d 常规剂量维持。
(5)并发症处理:以AMI、恶性心律失常或者心脏骤停等急症为表现的CASS 应及时对症抢救。
2、稳定期治疗
(1)CCB 是疗效最肯定且应用最广泛的防治CASS 的药物:地尔硫卓、硝苯地平(缓释或控制制剂)、氨氯地平、贝尼地平
(2)硝酸酯类
(3)钾通道开放剂:尼可地尔,5-10mg,tid
(4)他汀类药物
(5)抗血小板治疗:阿司匹林。ACS时双联抗血小板治疗
五、β受体阻滞剂如何应用?
(1)对于冠状动脉无显着狭窄的CASS 患者禁忌单独使用。
(2)对于合并有冠状动脉器质性狭窄或严重心肌桥,且临床主要表现为劳力性心绞痛的患者,若CCB和硝酸酯类疗效不佳时可以慎重联合使用高选择性β 阻滞剂。
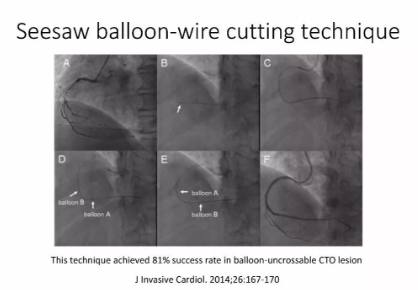
六、介入治疗
(1)经皮冠状动脉介入治疗CASS 患者原则上不主张介入治疗,个案报告显示,中重度冠状动脉狭窄基础上合并CAS 者可能从介入治疗中获益。
(2)对于因CAS 诱发的持续性室性心动过速或心室颤动等所导致的心脏骤停存活患者中,在规范药物治疗下仍反复发作者,可在进行充分评估的基础上考虑安装埋藏式自动除颤起搏器(ICD)。
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#痉挛#
36
挺好的,受教了
77
可以学习很多
77
好
76
收藏了非常好的文章
72
学习了,谢谢
75