Sci Transl Med:牙龈疾病与骨质疏松有什么关系?
2018-10-20 小通 生物通
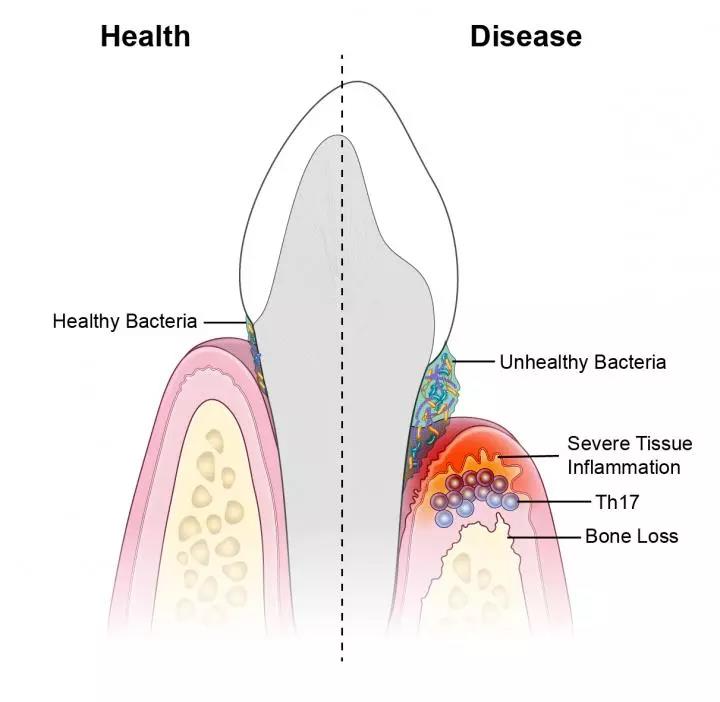
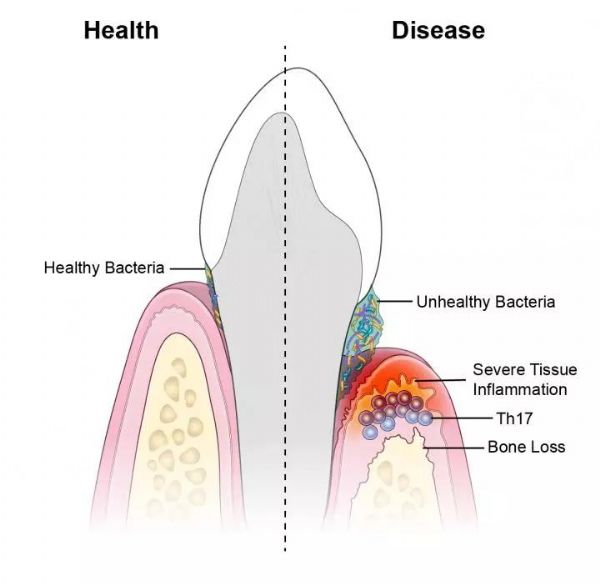
根据一项在小鼠和人身上进行的新研究,口腔中不健康的微生物群触发了炎症以及破坏组织中的特异性免疫细胞,导致与严重牙龈疾病相关的骨质丢失。
根据一项在小鼠和人身上进行的新研究,口腔中不健康的微生物群触发了炎症以及破坏组织中的特异性免疫细胞,导致与严重牙龈疾病相关的骨质丢失。
该项目由美国国立卫生研究院国立口腔与颅面研究所和美国宾西法尼亚大学牙医学院的研究人员领导可能会对新的治疗方法产生影响。该项研究在Science Translational Medicine杂志上面发表。
牙周病是一种常见的疾病,它影响着近一半的30岁以上的美国成年人和70%的65岁以上老人。在那些受到影响的病人中,细菌触发了牙齿周围组织的炎症,这可能导致牙周炎晚期阶段骨骼和牙齿流失。
“多年来我们都知道微生物会刺激炎症。通过刷牙和牙齿护理去除细菌可以控制炎症,但不是永久性的,这表明还有其他因素在起作用,”该文章的通讯作者国立口腔与颅面研究所(NIDCR)的临床研究人员Niki Moutsopoulos博士说,“我们的结果表明,被称为辅助性T细胞17的免疫细胞是这一过程的驱动力,提供了口腔细菌和炎症之间的联系。”
Moutsopoulos及其同事观察到,辅助性T细胞(Th)17在牙周炎患者的牙龈组织中比在健康人的牙龈组织中更普遍,并且Th17细胞的数量与疾病的严重程度相关。Th17细胞通常生活在所谓的屏障部位,如口腔、皮肤和消化道,在那里细菌首先与身体接触。Th17细胞是已知的,以防止口腔口疮,口腔真菌感染,但它们也与炎症性疾病,如牛皮癣和结肠炎有联系,表明它们在健康和疾病中发挥双重作用。
为了更好地理解这一动态,NIDCR的科学家与资深作者George Hajishengallis博士领导的宾夕法尼亚大学牙科医学院团队以及国立卫生研究院过敏反应和传染病研究所(NIAID)和美国立癌症研究所(NCI)进行合作。
科学家发现,与人类相似,与作为对照组的健康小鼠相比,患牙周炎的小鼠牙龈中积累了更多的Th17细胞。为了研究口腔微生物是否是Th17细胞积累的触发因素,研究人员对小鼠进行鸡尾酒式的广谱抗生素处理。他们发现,消除口腔微生物可防止牙周炎小鼠牙龈中Th17细胞的增加,同时使其他免疫细胞不受影响,提示不健康的细菌群会触发Th17细胞的积累。
接着,研究组想知道阻断Th17细胞是否可以减轻牙周病。当科学家用基因工程方法改造小鼠使其缺少Th17细胞,或者给这些动物注射一种阻止Th17细胞发育的小分子药物时,他们看到了类似的结果:牙周炎骨质流失减少。RNA分析表明,Th17阻断药物导致炎症、组织破坏和骨质流失相关基因的表达减少,提示Th17细胞可能在牙周炎中介导这些过程。
最后,研究人员在美国国立卫生研究院临床中心对35名基因缺陷导致他们缺乏Th17细胞的患者进行了研究。科学家们推断,如果像动物研究那样,Th17细胞对牙周炎很重要,那么没有Th17细胞应该能防止牙龈疾病。这确实是研究小组所发现的——与年龄和性别匹配的志愿者相比,患者对疾病的易感性更低,炎症和骨质流失更少。
“我们的临床观察表明我们的动物实验与人类相关,并提供进一步的证据证明Th17细胞是牙周炎的驱动力。”NIDCR的研究人员,该文章的第一作者,Nicolas Dutzan博士说。
“这些结果为牙周病的发病机制提供了重要的见解。”NIDCR主任Martha J. Somerman博士说,“重要的是,他们也提供了令人信服的证据来治疗靶向特定细胞,这可能最终帮助我们为患有该常见病的病人提供更好的治疗和更多的救济。”
原始出处:Dutzan N, Kajikawa T, Abusleme L, et al. A dysbiotic microbiome triggers TH17 cells to mediate oral mucosal immunopathology in mice and humans. Sci Transl Med. 2018 Oct 17;10(463).
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#Transl#
28
#TRA#
24
#骨质#
22
#Med#
30
学习了
71
学习了
49