Brit J Cancer:高强度间歇训练对睾丸癌幸存者疲劳和生活质量影响研究
2018-05-13 AlexYang MedSci原创
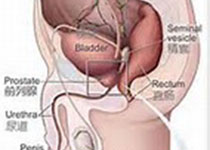
睾丸癌幸存者(TCS)处于癌症相关疲劳、心理障碍和生活质量相关的心理障碍(HRQoL)风险增加的情况中。最近,研究人员调查了高强度的间歇训练(HIIT)在TCS患者中对病人报道的结果(PROs)的影响。之后,研究人员探索了心肺功能作为干预效果的一个调节标记,并挑选了干预效果调节标记的基线特性。研究包括了63名TCS患者,并且随机分配到监督下的HIIT组或者常规护理组中。并在基线点、干预后和跟踪调查
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#高强度间歇训练#
40
学习了谢谢分享
47
#疲劳#
30
#睾丸#
28
#高强度#
35
不错
48