Allergy Asthma Proc:常年性变应性鼻炎患者奥洛他定-莫米松组合鼻喷雾的长期安全性和效果研究
2019-07-11 AlexYang MedSci原创
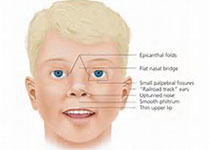
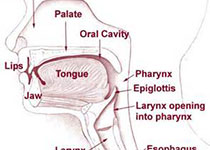
最近,有研究人员调查了GSP301鼻喷雾的安全性和效果,具体是详细调查了GSP301在常年性变应性鼻炎患者(PAR)中的长期(52周)安全性和效果情况。研究是一个随机、双盲和平行的研究,包括了601名PAR患者(年龄不小于12岁),并按章4:1:1的比例随机分配到1天2次GSP301(奥洛帕他定665毫克和莫米松25微克[pH 3.7])或者2种GSP301药物处方(安慰剂pH3.7或者7.0)。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#asthma#
47
#AST#
38
#长期安全性#
56
#ROC#
47
#莫米松#
43
#变应性鼻炎#
41
#ALL#
34
#PRO#
30
疗效只是效果的众多方面之一,还要看对患者的获益,包括生活质量等因素共同决定效果的
41