Crit Care:非ST段抬高型心肌梗死患者闭塞的犯罪动脉患病率和结局分析!
2018-02-09 xing.T MedSci原创
由此可见,大部分是NSTEMI人群为OCA患者。这些患者表现出更严重的症状和更差的临床结局。这些患者是否应该采取更积极的治疗策略还有待进一步研究。
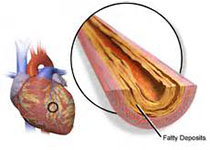
近日,危重病医学领域权威杂志Critical Care上发表了一篇研究文章,研究人员旨在明确非ST段抬高心肌梗死(NSTEMI)患者闭塞的犯罪动脉(OCA)患病率和影响。
研究人员检索了PubMed、EMBASE和Web of Science等数据库,不受任何语言限制,检索时间截止至2016年7月1日。NSTEMI成人的观察性队列或临床试验具有资格入组,以确定OCA在冠状动脉造影术中的比例。如果报告了OCA与临床终点之间的关联的研究,则进一步纳入分析以确定对结局的影响。
在纳入的25项NSTEMI患者的研究中,有8812例患者发生OCA。NSTEMI患者中OCA的平均比例为34%(95%可信区间为30-37%)。OCA患者更可能以左旋动脉为犯罪动脉(比值比(OR)为1.65,95%可信区间为1.15-2.37,P=0.007),与非闭塞性犯罪动脉相比,左旋动脉作为犯罪动脉与较低的左心室射血分数(标准差为-0.29,95%可信区间为-0.34至-0.34,P<0.001)、较高的酶峰值水平(标准差为0.43,95%可信区间为0.27-0.58,P<0.001)和较高的心源性休克风险(OR为1.66,95%可信区间为1.35-2.04,P<0.001)相关。OCA患者的死亡率(OR为1.72,95%可信区间为1.49-1.98,P<0.001)和复发性心肌梗死(OR为1.7,95%可信区间为1.06-2.75,P=0.029)也高于非闭塞性犯罪动脉患者。
由此可见,大部分是NSTEMI人群为OCA患者。这些患者表现出更严重的症状和更差的临床结局。这些患者是否应该采取更积极的治疗策略还有待进一步研究。
原始出处:
Chi-Sheng Hung,et al. Prevalence and outcome of patients with non-ST segment elevation myocardial infarction with occluded “culprit” artery–a systemic review and meta-analysis.Critical Care.2018. https://doi.org/10.1186/s13054-018-1944-x
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#非ST段#
31
#非ST段抬高#
33
#非ST段抬高型#
40
#非ST段抬高型心肌梗死#
28
#患病率#
20
#ST段抬高#
33
#ST段#
39
v还好还好很久很久
61
一起学习学习
54
学习了受益匪浅
51