2019年美国临床内分泌学家协会(AACE)大会:Teprotumumab治疗甲状腺眼病的III期试验结果
2019-04-13 不详 网络
Horizon制药公司近日宣布将在2019年美国临床内分泌学家协会(AACE)大会上公布III期临床试验(OPTIC研究)的最新结果,该研究评估了teprotumumab治疗活动性甲状腺眼病(TED)的有效性和安全性。
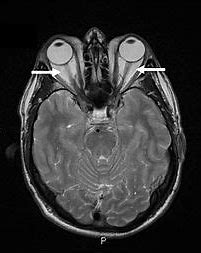
Horizon制药公司近日宣布将在2019年美国临床内分泌学家协会(AACE)大会上公布III期临床试验(OPTIC研究)的最新结果,该研究评估了teprotumumab治疗活动性甲状腺眼病(TED)的有效性和安全性。甲状腺相关眼病是成年人最常见的眼眶病之一,属于自身免疫性疾病。大多数患者可有甲状腺功能异常表现,但即使在甲状腺功能正常的情况下,也可能发生TED。
Teprotumumab是全人源单克隆抗体(mAb),为胰岛素样生长因子1受体(IGF-1R)的靶向抑制剂。Teprotumumab是一种研究性药物,其安全性和有效性尚未确定。OPTIC验证性临床研究在美国、德国和意大利的主要中心进行。除OPTIC试验外,Horizon正在进行OPTIC-X延伸试验,以进一步深入了解Teprotumumab的长期疗效和安全性。
原始出处:
http://www.firstwordpharma.com/node/1634957#axzz5kmtmGZrh
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#分泌#
39
#甲状腺眼病#
57
#ACE#
32
#临床内分泌#
40
#II期试验#
36
#III#
50
#mAb#
30
#眼病#
37
#III期#
39
#Teprotumumab#
43