Nat Cell Biol:重磅!可能用于胰腺癌治疗新方法
2017-04-19 枫丹白露 medicalxpress
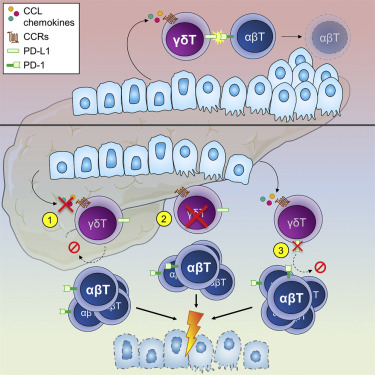
【什么促使胰腺癌细胞如此活跃?】胰腺癌是最具侵袭性的肿瘤类型之一,因为它早期开始形成转移。然而,癌症本身通常只被发现得很晚,进而导致了较高的病人死亡率。弗里德里希亚力山大大学(FAU)的研究人员现在已经发现为什么胰腺癌和其他恶性肿瘤类型可以如此迅速地传播。研究结果现已发表在著名的《自然细胞生物学》杂志上。由Thomas Brabletz博士和实验医学主席Marc Stemmler博士领导的FAU研
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#治疗新方法#
30
#新方法#
24
#Bio#
25
#Nat#
21
#Biol#
25
#CEL#
21
#Cell#
19
#重磅#
21