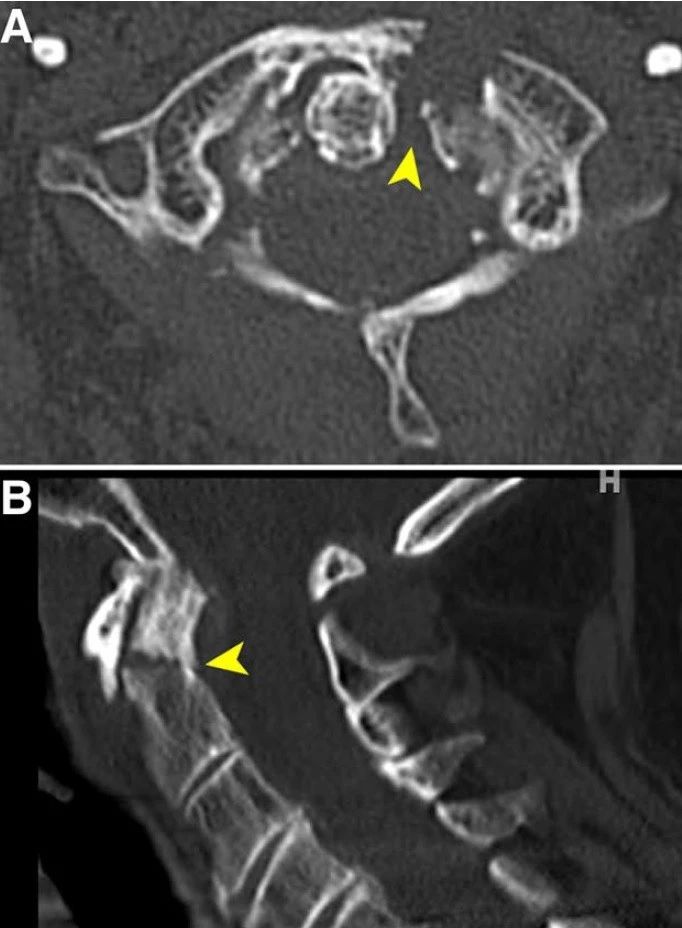
双侧胫骨骨内腱鞘囊肿1例
2019-02-15 侯跃超 中国实验诊断学
骨内腱鞘囊肿是骨的良性病变,临床上多为单发,多发病例少见,临床表现为病变部位的慢性疼痛,缺乏特异性,为进一步加强对本病的认识,本文对我院收治的1例患者进行报道并文献复习。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#骨内腱鞘#
30
没影像资料,不直观!
77
#囊肿#
25
#胫骨#
35
#双侧#
36