Radiology:MR成像涉足新领域--评价COPD患者局部肺通气的价值
2017-11-15 shaosai MedSci原创
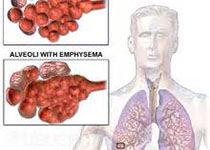
本研究旨在利用自由呼吸动态19F-气体磁共振(MR)成像在慢性阻塞性肺疾病患者中局部肺通气的定性评价,并将结果发表在Radiology上。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








又一新的检查方法 看好
50
#局部#
31
#评价#
28
#COPD患者#
33
学习了.好文章
53
本研究表明.利用1.5TMR扫描仪.动态19F气体廓清MR成像在自由呼吸条件下定量评估局部肺通气是可行的.甚至是在阻塞性肺节段.
45