Cancer Cell:TMB标志物显神威!可增加小细胞肺癌I-O治疗有效性
2018-05-15 月下荷花 肿瘤资讯
CheckMate032研究表明,小细胞肺癌(SCLC)可获益于免疫检查点抑制治疗,但哪些患者在免疫治疗中获益更多并不清楚。近日美国Hellmann教授在Cancer Cell杂志发表了CheckMate032的回顾性研究,结果表明高肿瘤突变负荷(TMB)SCLC患者从纳武利尤单抗(nivolumab)联合伊匹木单抗(ipilimumab)治疗中获益最大。
CheckMate032研究表明,小细胞肺癌(SCLC)可获益于免疫检查点抑制治疗,但哪些患者在免疫治疗中获益更多并不清楚。近日美国Hellmann教授在Cancer Cell杂志发表了CheckMate032的回顾性研究,结果表明高肿瘤突变负荷(TMB)SCLC患者从纳武利尤单抗(nivolumab)联合伊匹木单抗(ipilimumab)治疗中获益最大。
研究背景
小细胞肺癌占所有肺癌10%–15%,大约75%患者为广泛期。标准一线治疗为含铂化疗,一旦疾病进展则缺少有效治疗,预后极差。纳武利尤单抗为免疫检查点抑制剂,无论是单药还是与伊匹木单抗联合治疗既往接受过治疗的SCLC,均可获得持续治疗反应,延长生存。CheckMate 032研究中,纳武利尤单抗单药治疗进展期SCLC的2年生存率14%,与伊匹木单抗联合为26%,因此NCCN指南推荐纳武利尤单抗±伊匹木单抗作为SCLC的二线或二线以上治疗。
然而一直缺少有效预测SCLC免疫检查点抑制治疗有效性的标志。与其它肿瘤不同,SCLC较少表达程序化死亡配体1(PD-L1),而且无论有无PD-L1表达,纳武利尤单抗±伊匹木单抗治疗均可能有效。多数SCLC与吸烟有关,因此SCLC特征之一是高体突变负荷。其它实体肿瘤中已显示高TMB与免疫检查点抑制治疗有效性相关,但在SCLC中是否也存在这种关系并不清楚。
研究方法
CheckMate032研究中接受纳武利尤单抗单药(3mg/kg,每2周一次)或纳武利尤单抗+伊匹木单抗(1mg/kg+3mg/kg,每3周一次,共4周期,然后纳武利尤单抗3mg/kg,每2周一次)联合治疗的SCLC患者进行全外显子测序。TMB定义为错义体突变总和,采用三分位法将TMB分为低负荷<143突变,中等负荷143-247突变,高负荷≥248突变。
研究结果
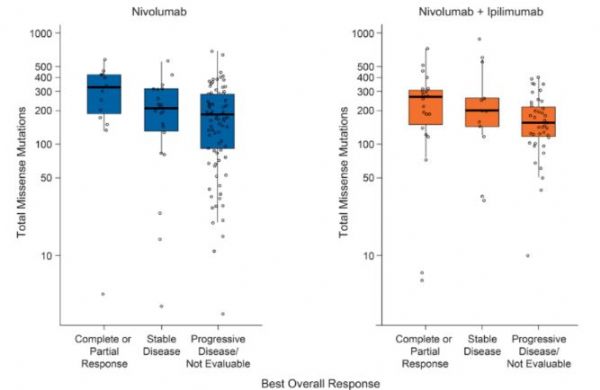
结果表明纳武利尤单抗单药和纳武利尤单抗+伊匹木单抗联合治疗,高TMB患者的客观反应率(21.3%和46.2%)高于低(4.8%和22.2%)和中(6.8%和16.0%)TMB患者(图1),所有患者纳武利尤单抗+伊匹木单抗联合治疗的客观反应率高于纳武利尤单抗单药治疗(图1)。无论是联合还是单药治疗,获得完全或部分反应患者的TMB高于疾病稳定或疾病进展的患者(图2)。
纳武利尤单抗单药和纳武利尤单抗+伊匹木单抗联合治疗,高TMB患者的1年无进展生存率(21.2%和30.0%)高于低(不能计算和6.2%)中(3.1%和8.0%)肿瘤突变患者,高TMB患者联合治疗的1年无进展生存率优于单药治疗(图3),低中TMB患者联合治疗与单药治疗无差异,总生存结果与之相似(图4)。总之,高TMB增加纳武利尤单抗和纳武利尤单抗+伊匹木单抗有效性,纳武利尤单抗+伊匹木单抗的临床获益超过纳武利尤单抗单药。

图1 TMB与客观反应率
图2 个体最佳治疗反应与TMB
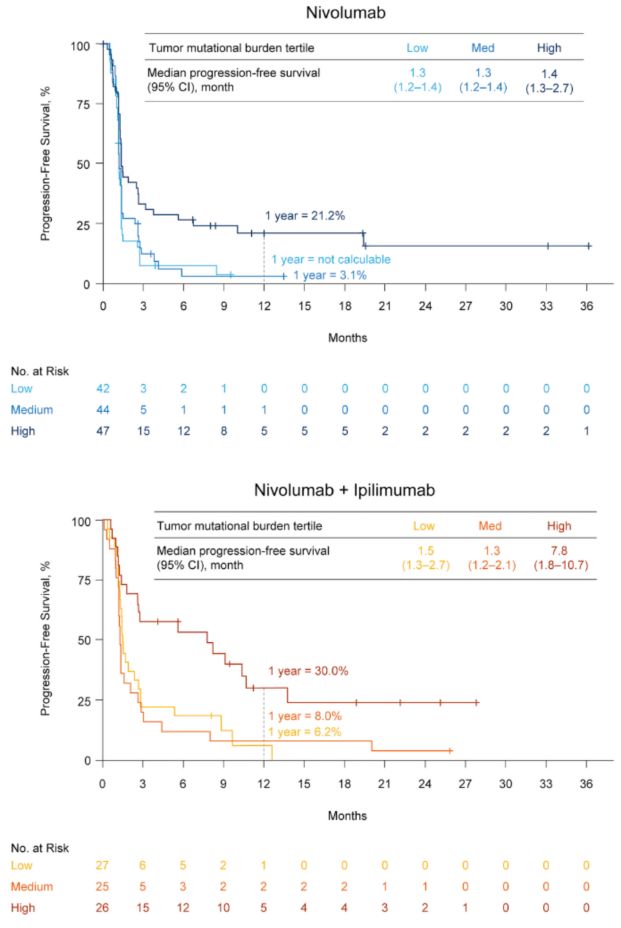
图3 治疗、TMB与无进展生存
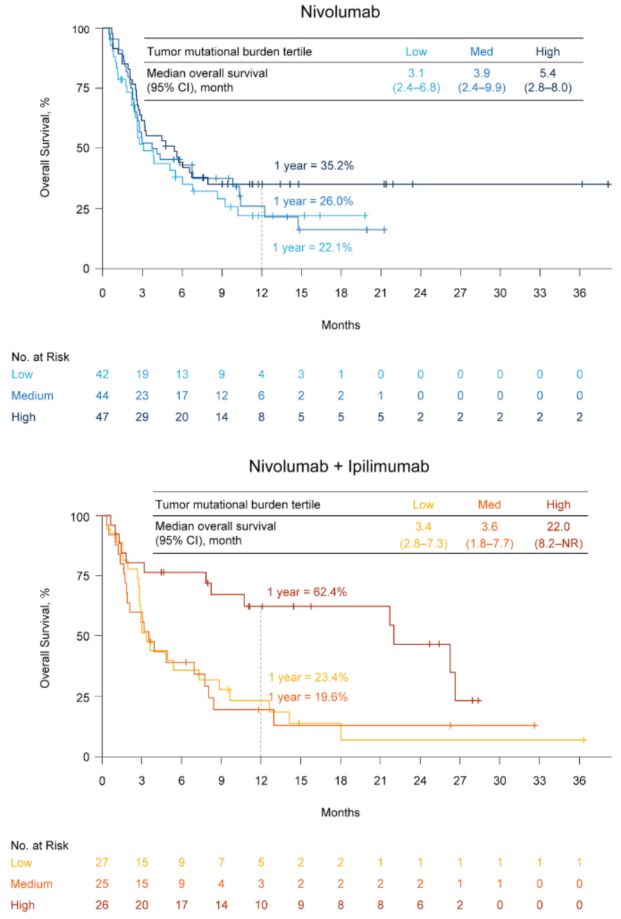
图4治疗、TMB与总生存
结果讨论与展望
这项研究评估了SCLC的TMB与免疫检查点抑制治疗有效性的关系,结果表明高TMB患者较低中TMB患者从纳武利尤单抗和纳武利尤单抗+伊匹木单抗治疗中获益更多,这与纳武利尤单抗治疗非小细胞肺癌(NSCLC)和尿路上皮癌、伊匹木单抗治疗黑色素瘤的结果相似,因此TMB可能也是SCLC免疫检查点治疗反应的预测标志。
初始观察发现虽然纳武利尤单抗+伊匹木单抗联合治疗SCLC能增加获益,但较纳武利尤单抗单药治疗的毒性更大,因此确定单药或联合治疗的不同预测标志十分必要。这项研究发现,SCLC患者伴高TMB时,纳武利尤单抗+伊匹木单抗联合治疗的生存远超过历史对照,中低TMB患者联合治疗的客观反应率虽较单药改善,但无进展生存和总生存并无差别。结果提示高TMB患者,联合治疗获益优于单药治疗,而中低TMB患者单药治疗也许是最佳选择。
这项研究表明,TMB对SCLC免疫治疗反应有预测作用,但尚不清楚其分子多样性是否足以区分免疫治疗反应不同的临床亚组,目前只能得出负荷最高者免疫治疗获益最多。
有人认为突变负荷分析并不可行,因为SCLC标本取材多为小标本且存在较多坏死组织。但这项研究显示,61%患者的活检组织足以用于全外显子检测,因为是回顾性研究,活检取材时并未预先计划全外显子检测,若事先计划全外显子检查则取材合乎标准的患者比例可能更高。总之这项研究证实,SCLCTMB检测可行,如若为前瞻性研究则可获更高的成功率。
目前不清楚TMB和纳武利尤单抗+伊匹木单抗治疗结果之间究竟如何产生联系。有假说认为,加入伊匹木单抗增加抗肿瘤T细胞克隆储备,同时也降低TMB的预测相关性。但这个假说似乎与SCLC无关,因为TMB在SCLC中是纳武利尤单抗+伊匹木单抗治疗反应增加的预测标志。与之相似,有研究显示NSCLC采用纳武利尤单抗+伊匹木单抗联合治疗的反应进一步改善。需要更多研究明确二者协同作用的潜在免疫学机制。
研究还发现,不论是均分法、三分法还是四分法,皆显示高TMB与结果改善相关,说明SCLC的TMB与免疫治疗获益的关系很稳定,同时也提示多个阈值均可富集获益人群,需要进一步优化,也要更好地理解增加免疫原性的体突变分子特征。目前另有二个评估纳武利尤单抗±伊匹木单抗治疗SCLC有效性的III期研究(CheckMate331和CheckMate451),这二项研究会有更多数据明确TMB与治疗结果间的关系。
总之,SCLC患者采用纳武利尤单抗单药或纳武利尤单抗+伊匹木单抗联合治疗时,高TMB能增加治疗有效性,其中以联合治疗的临床获益更多,联合治疗的1年生存率几乎是单药治疗的2倍。高TMBSCLC患者接受免疫联合治疗时,无进展生存和总生存改善尤其显着,这与NSCLC的数据相似,提示TMB可能是所有肺癌免疫治疗的潜在生物学标志。
原始出处:Hellmann MD, Callahan MK, Awad MM, et al. Tumor Mutational Burden and Efficacy of Nivolumab Monotherapy and in Combination with Ipilimumab in Small-Cell Lung Cancer. Cancer Cell. 2018 Apr 21.
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言






#TMB#
30
#cancer cell#
26
#标志物#
29
#Cell#
37
#CEL#
36
TMB的诊断作为PD-1/L1药物的伴随诊断在SCLC患者中更合适
74
学习了.长知识
64