ESH2018丨ASCOT LEGACY研究:高血压患者长期全因死亡率及心血管死亡率的决定因素
2018-06-17 国际循环编辑部 国际循环
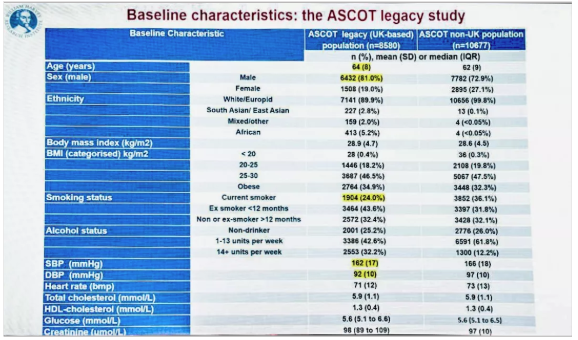
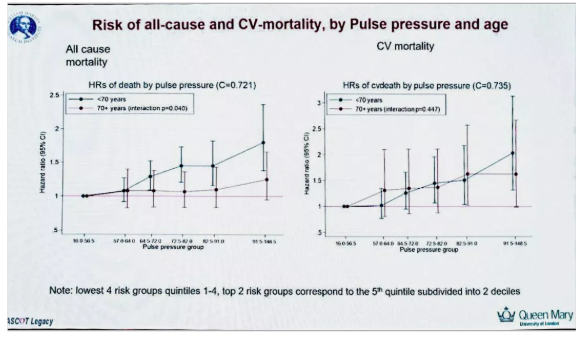
西班牙巴塞罗那当地时间2018年6月9日上午,在ESH 2018年会最新研究专场上,来自英国伦敦玛丽女王大学的A.Gupta教授分享了ASCOT LEGACY研究16年随访的最新结果,揭秘了高血压患者长期全因死亡率及心血管死亡率的决定因素。

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#ASC#
54
#决定因素#
49
#全因死亡率#
41
#心血管死亡率#
50
#高血压患者#
47
#ESH#
33
#心血管死亡#
42
阅
67
学习了.长知识
65