室间隔完整的肺动脉闭锁低出生体重儿围术期麻醉管理1例
2019-04-19 郁丽娜 薛瑛 王晟 麻醉安全与质控
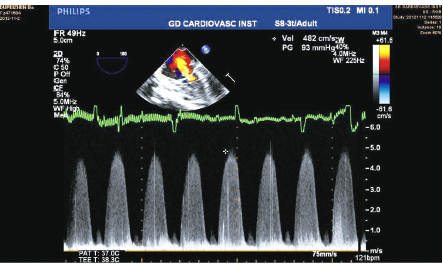
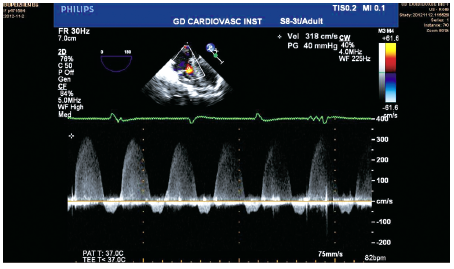
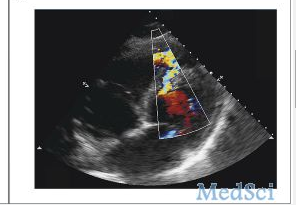
患儿,女,因“母亲双胎妊娠35周、疤痕子宫、重度子痫前期”行剖宫产娩出后,转入新生儿科。娩出时羊水清,患儿1、5、10min的Apgar评分均10分,出生体质量为1870g。新生儿科查体:四肢脉搏血氧饱和度(SpO2)偏低(≤90%),心前区可闻及心脏杂音,床旁心脏超声示PA/IVS,动脉导管未闭(6mm),房间隔缺损(5mm,右向左分流),卵圆孔未闭(6.4mm,右向左分流),右心室发育不良,重
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#室间隔#
25
#围术期#
34
#出生体重#
29
#低出生体重#
29