ACC 2018:ARNI研究速递:沙库巴曲缬沙坦可能有助于改善心肌功能
2018-03-17 《国际循环》编辑部 国际循环
2018年3月10~12日,第67届美国心脏学学会年会(ACC 2018)在美国奥兰多盛大召开。关于心力衰竭新药血管紧张素受体脑啡肽酶抑制剂(ARNI)的研究进展成为一大亮点。其中,来自美国研究者的两篇研究报道了沙库巴曲缬沙坦对心肌功能的影响,引起广泛关注。我刊摘取精华内容,并特邀南京医科大学第一附属医院李新立教授进行精彩点评。
2018年3月10~12日,第67届美国心脏学学会年会(ACC 2018)在美国奥兰多盛大召开。关于心力衰竭新药血管紧张素受体脑啡肽酶抑制剂(ARNI)的研究进展成为一大亮点。其中,来自美国研究者的两篇研究报道了沙库巴曲缬沙坦对心肌功能的影响,引起广泛关注。我刊摘取精华内容,并特邀南京医科大学第一附属医院李新立教授进行精彩点评。
研究一
PARAMOUNT试验:沙库巴曲缬沙坦改善HFpEF患者的左心室心肌形变能力
美国布莱根妇女医院Tor Biering-Sorensen博士报道了PARAMOUNT研究的一项新分析,评估了沙库巴曲缬沙坦对射血分数保留的心力衰竭(HFpEF)患者左心室心肌形变能力的影响。该新分析选取基线及36周时均具有高质量二维斑点追踪成像质量的患者(沙库巴曲缬沙坦组60例,缬沙坦组75例),评估其左心室心肌整体纵向应变(GLS)和整体圆周应变(GCS)自基线至36周的变化。
结果显示,在36周时,沙库巴曲缬沙坦组患者心肌GCS较缬沙坦组显著改善(Δ4.42,95%CI:0.67~8.17,P=0.021),两组之间GLS差异无统计学意义(Δ0.25,95%CI:-1.19~1.70,P=0.73)(图1)。
研究者得出结论,在HFpEF患者中,沙库巴曲缬沙坦治疗36周可较缬沙坦显著改善左心室心肌整体圆周应变。
图1.PARAMOUNT研究:沙库巴曲缬沙坦改善HFpEF患者心肌整体圆周应变
李新立教授点评:PARAMOUNT研究为HFpEF治疗带来新希望
PARAMOUNT研究的这项分析观察了HFpEF患者左心室心肌形变能力,以GCS和GLS作为评估指标。心肌的圆周应变表示心脏短轴方向的环形运动,GCS降低表示心肌缺血累及至中间层,能在一定程度上反映心肌缺血的严重性。沙库巴曲缬沙坦显著改善GCS的结果提示其可在一定程度上改善心肌缺血。GLS则主要反映心脏在长轴方向的收缩功能,本研究中沙库巴曲缬沙坦较缬沙坦对GLS有改善趋势,具体机制有待将来进一步研究。
临床心衰患者中的近半数者得以保留正常或接近正常的射血分数,但对于HFpEF患者,目前尚无任何治疗方案可降低病死率和改善预后,HFpEF的治疗仍属世界性难题。PARAMOUNT研究无论是主要终点还是其他指标均显示出沙库巴曲缬沙坦对HEpEF患者的有益作用,结果包括:改善NT-proBNP水平,减小左心房体积,以及改善左心室心肌形变能力。尽管PARAMOUNT是Ⅱ期临床研究,但其结果的确为我们带来了新希望。正在进行中的以心血管疾病和死亡率为硬终点的临床试验——PARAGON-HF研究,将进一步探索沙库巴曲缬沙坦在HEpEF人群中是否优于血管紧张素受体拮抗剂以及与缬沙坦相比的安全性。
研究二
ARNI促进心肌早期血管生成,并改善心肌灌注,抑制心肌梗死后重构
为探索沙库巴曲缬沙坦对心肌血管生成及灌注的影响,耶鲁大学医学院Stephanie L.Thorn博士等开展了一项实验研究。结果显示,在大鼠急性心肌梗死模型中,沙库巴曲缬沙坦治疗1周可改善梗死心肌99mTc-NC100 692的摄入(图2A);治疗5周可显著增加多巴酚丁胺负荷试验诱导201铊摄入(图2B)以及减少梗死周边心肌细胞的体积增加(图2C);而且,治疗5周后,沙库巴曲缬沙坦治疗可预防梗死周边心肌细胞肥大,并增加毛细血管密度(图2D)。
研究者得出结论,在急性心肌梗死动物模型中,沙库巴曲缬沙坦治疗可促进早期血管生成,改善心肌灌注,并减少心肌重构。
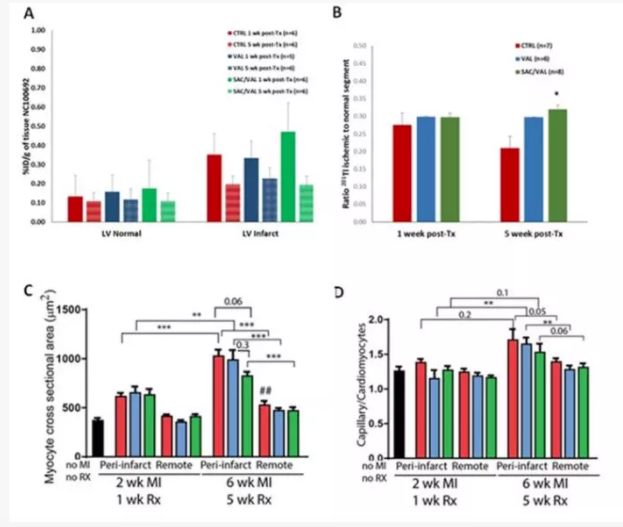
图2.动物实验:沙库巴曲缬沙坦治疗促进早期血管生成,改善心肌灌注,并减少心肌重构
李新立教授点评:沙库巴曲缬沙坦改善心肌功能或为探索其更广泛心血管作用提供新思路
尽管这是项动物研究,但其结果提示沙库巴曲缬沙坦可能从根本上针对缺血性心脏病的病理生理机制进行治疗,包括促进梗死后心肌早期血管生成、改善心肌灌注、抑制心肌重构等。这为我们后续开展相关临床试验奠定了实验依据,为探索该药的心血管保护作用提供了新的策略,带来了新的思路和希望。
本届ACC报道的两项新研究均提示沙库巴曲缬沙坦可能对心肌有改善作用,而心肌功能涉及心力衰竭、心肌梗死等多种心脏疾病,这也提示我们该药在心血管疾病治疗中可能发挥更多作用。目前沙库巴曲缬沙坦已在中国上市,用于治疗射血分数降低的心力衰竭(HFrEF)患者。但实际上,在该药的里程碑性研究PARADIGM-HF中,约60%为缺血性心脏病导致的HFrEF患者,在这样的人群中沙库巴曲缬沙坦较ACEI可进一步降低主要终点(心血管死亡和心衰住院)风险20%,其实也从另一个角度印证了其对心肌缺血性疾病的有益作用。
究其机制,沙库巴曲缬沙坦是首个血管紧张素受体脑啡肽酶抑制剂(ARNI),在抑制脑啡肽酶的同时,阻断血管紧张素Ⅱ的1型受体,两个成分协同作用较单纯的RAS抑制剂(ACEI/ARB)作用更完善,是其临床更多获益的主要原因。随着研究的不断深入,沙库巴曲缬沙坦的更多机制将被挖掘出来,包括这两项新研究所提示的改善心肌功能作用,这都可能是其心血管获益的机制之一。
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#ACC#
29
#缬沙坦#
26
#沙库巴曲缬沙坦#
50
#ARNI#
54
学习了受益匪浅
59
了解一下.谢谢分享!
60