你心里的那个“她”会是谁?
2018-05-23 人间世 医学界心血管频道
大家对心脏的大体解剖应该都有一个概念,简单来说心腔里除了瓣膜,总体还是“空荡荡的”,从超声上看心腔里只有瓣膜在那里荡着秋千,此外就是黑乎乎一片。
大家对心脏的大体解剖应该都有一个概念,简单来说心腔里除了瓣膜,总体还是“空荡荡的”,从超声上看心腔里只有瓣膜在那里荡着秋千,此外就是黑乎乎一片。
但是有些人的心里总会多了一个"她",今天我们来看看这个"她"可能会是谁?
病例简介~
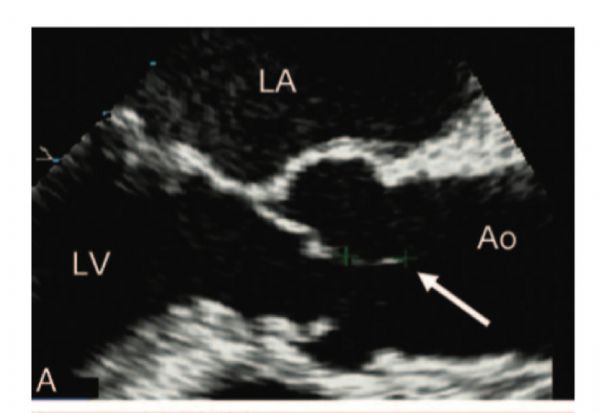
患者69岁女性,主因二尖瓣狭窄和冠心病住院行外科手术治疗,术前超声心动示二尖瓣狭窄、主动脉瓣反流,余未见异常。术中食道超声也证实了术前的瓣膜病变,但是却发现了一个不速之客(见图1),主动脉瓣上有一个发丝样强回声结构,长约10mm,呈飘带样活动。我想大家都会猛然出一身冷汗,这是什么鬼?
图1. 食道超声示主动脉瓣上发丝样强回声结构
一般而言,心脏瓣膜上出现附着物,我们需要在血栓、赘生物和肿瘤这三大常见病因中鉴别:
血栓:根据Virchow三要素理论,血栓多见于低速流动的血液状态,所以瓣膜血栓也好发于合并室壁运动异常或心室自发性显影的患者,超声图像的特点是类圆形实性回声,且与瓣膜间无蒂相连。
肿瘤:心脏瓣膜最常见的肿瘤是乳头状纤维弹性瘤,一般没什么特别的症状,多为偶然发现,超声上多表现为团块状,一般起自瓣叶中部,与瓣膜通过蒂相连。另外比较常见的就是粘液瘤,它最大的特点是通过蒂与心内膜相连,活动度非常大,可影响瓣膜的开启和关闭,其次粘液瘤通常含有肉芽组织,容易出现小面积出血和钙化,其回声一般不均匀。
回到该病例,患者无感染性心内膜炎临床征象,也无血栓形成倾向,超声图像也并不符合常见良性肿瘤的特点,那它会是什么呢?本着外科医生的果断和利落,他们在完成预定的瓣膜置换和搭桥手术的同时,顺带切除了这个“东西”,结果见图2。
图2.手术切除的病理标本
随后的病理结果告诉我们,这个奇怪的结构是兰伯氏赘生物(Lambl’sexcrescene )。它是由捷克医师Lambl在1856年第一次描述而得名。其组织学特点是表面有单层内皮细胞覆盖,与瓣膜本身的内皮细胞层相延续,中央核通常是无细胞的结缔组织基质。
关于兰伯氏赘生物的形成机制,目前并不是很清楚,有一种理论认为是由于瓣膜处心内膜受损引起。随着瓣叶长期连续拍击,心内膜面会出现细小的磨损和撕裂,损伤处继发纤维沉积,继而单层内皮细胞将纤维结缔组织覆盖形成兰伯氏赘生物。
至于兰伯氏赘生物的临床意义尚无定论,有些人认为属于正常衰老性改变,但是有研究显示兰伯氏赘生物可能脱落或继发血栓形成,也许是一部分隐源性卒中的病因。因此对于它的处理措施也缺乏共识,有学者建议,无症状者可密切观察,有过1次脑血管事件者,建议抗凝治疗,如果复发可考虑手术切除。
心脏瓣膜附着物中,大家最熟悉的应该是感染性心内膜炎引起的赘生物了,但是大家也一定不要忘了另外两个常见的病因,当然在常见的病因排除后,也要记得这细如发丝的“她”。
原始出处:
[1]Nakahira J, et al. Lambl’s Excrescence onAortic Valve Detected by Transesophageal Echocardiography. Anesth Analg.2008;106(6):1639-40.
[2] Chu A, et al. Lambl's Excrescence Associatedwith Cryptogenic Stroke: A Case Report and Literature Review. Am J Case Rep 2015;16:876-81.
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








学习谢谢分享
63
学习了.谢谢分享
62
了解了解.学习学习
67
学习了感谢分享
78
好好好好好好好好
54