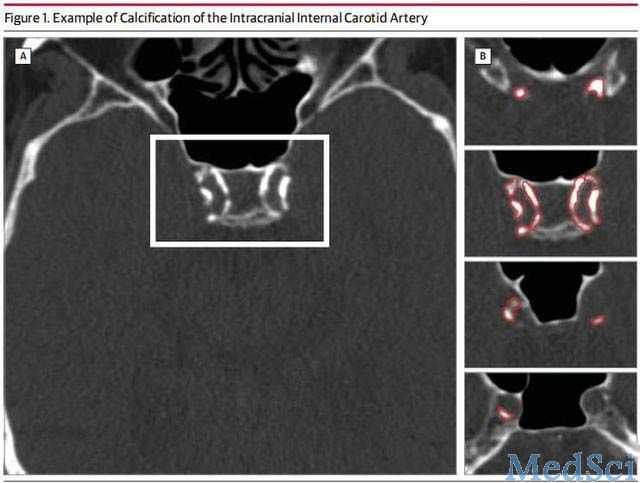
JAMA Neurol:颈内动脉颅内段粥样硬化增高卒中风险
2014-03-04 lighthouse dxy
动脉粥样硬化性脑梗死是缺血性卒中最常见的类型。其中,颈内动脉颅内段的粥样硬化被认为是40岁以上人群卒中的最重要危险因素,也是各种卒中防治手段的主要干预靶点。目前,关于白种人中颅内动脉粥样硬化对卒中影响的研究仍较有限。曾有报道发现,当以颈内动脉颅内段的钙化(ICAC)作为动脉粥样硬化的指标,有超过80%的白种人存在颅内动脉粥样硬化。近期,来自于荷兰鹿特丹伊拉姆斯医学中心的M. Arfan Ikram
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#粥样硬化#
29
#Neurol#
29
#卒中风险#
31
#增高#
38
#增高#
39
#颈内动脉#
40