糖尿病前期和早期怎么治?这才是“正确的打开方式”!
2018-07-08 佚名 医学界内分泌频道
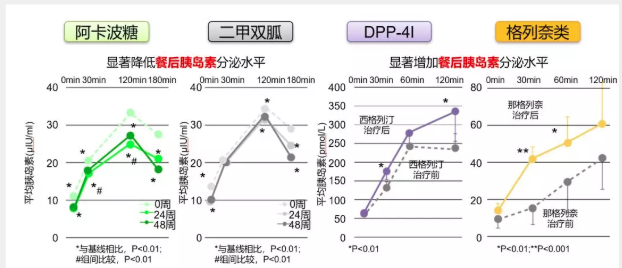
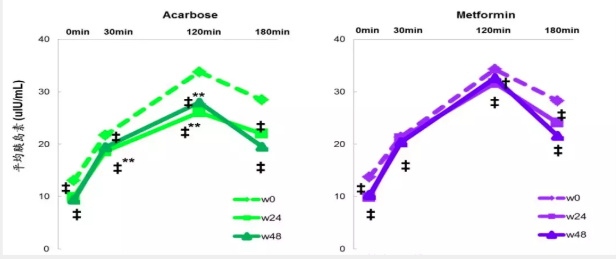
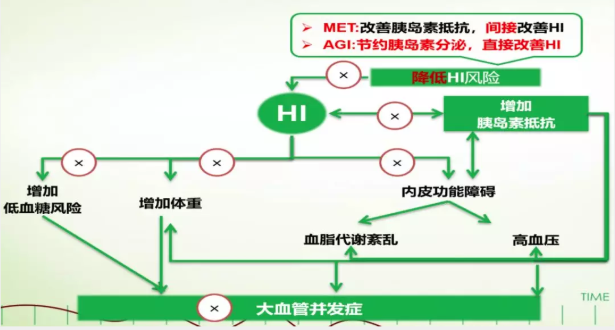
2018年6月22-26日,美国糖尿病学会(ADA)第78届年会在美国奥兰多拉开帷幕。在ADA拜耳高峰会上,华中科技大学同济医院附属协和医院陈璐璐教授担任大会主席,中日友好医院内分泌代谢中心主任杨文英教授和华中科技大学同济医学院附属同济医院内分泌科主任余学锋教授发表了精彩的主题演讲,就阿卡波糖在糖尿病前期、T2DM人群中的应用及获益进行了深入探讨。

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












很好.受益匪浅
54
学习了
64
学习了
68
糖尿病早期的治疗.
58
约你了
60
学习了
31
学习了.谢谢分享.
17
学习了
21
学习了
27