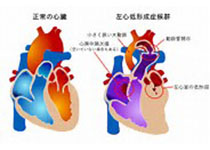
Heart:先天性心脏病相关肺动脉高压患者皮下曲前列环素疗效分析!
2018-02-08 xing.T MedSci原创
由此可见,皮下注射曲前列环素治疗总体安全有效,疗效至少持续12个月,可用于冠心病相关PAH患者的治疗。
近日,在心脏病领域权威杂志Heart上发表了一篇研究文章,研究人员旨在评估先天性心脏病(CHD)相关肺动脉高压(PAH)成年患者接受皮下曲前列环素治疗12个月的疗效和安全性。
研究人员对连续就诊的接受皮下曲前列环素至最大耐受剂量的成年CHD-PAH患者进行了观察性研究。
研究人员纳入了患有WHO III或IV级疾病的接受曲前列环素治疗的晚期CHD-PAH患者(n=32,年龄为40±10岁,20名女性),这些患者包含对波生坦治疗反应欠佳(n=12)的患者、WHO功能分类(FC,n=7)IV级疾病患者或在波生坦批准之前(n=13)的患者。在多元混合模型中,从基线至12个月的6分钟步行距离(6-MWD)平均增加114米(76-152)(P<0.001)。WHO FC显著改善(P=0.001),并且B型脑利钠肽从1259(375-2368)pg/mL降至380(144-1468)pg/mL(P=0.02)。在14例接受曲前列环素治疗前后血流动力学数据可用的患者中,肺血管阻力明显下降(从18.4±11.1降至12.6±7.9,P=0.003)。最常见的不良事件为输注部位红斑和疼痛。一名患者因治疗8个月后无法忍受输注部位疼痛而停止治疗。没有观察到其他主要的治疗相关并发症。早期随访时5例患者死亡,这些患者先前6-MWD有所下降。
由此可见,皮下注射曲前列环素治疗总体安全有效,疗效至少持续12个月,可用于冠心病相关PAH患者的治疗。
原始出处:
Nika Skoro-Sajer,et al. Subcutaneous treprostinil in congenital heart disease-related pulmonary arterial hypertension. Heart. 2018. http://dx.doi.org/10.1136/heartjnl-2017-312143
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#肺动脉高压患者#
29
#动脉高压#
41
#疗效分析#
30
#ART#
28
#先天性#
35
#HEART#
23
#曲前列环素#
48
肺动脉高压表面是罕见病,事实上临床上并不少见,治疗药物虽然有一些,但是整体仍然不理解,可能未来需要采用综合治疗措施。
50
好文章.学习了.
81