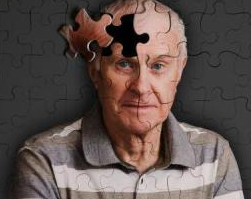
JAD:基因突变研究指出阿尔茨海默症病因新方向
2016-06-29 佚名 生物谷
来自澳大利亚阿德莱德大学的研究人员对可能引起早发阿尔茨海默症的基因突变进行了分析,为该病病因研究开辟了新的方向。 之前研究已经证明beta淀粉样蛋白出现异常积累是引起阿尔茨海默症的重要原因。但是也有研究人员对此表示担忧,认为上述情况并不能解释所有病因,并且至今没有开发出成功的治疗方法。阿德莱德大学的科学家们与澳大利亚其他大学的研究人员共同合作,通过一系列分析提出了关于PSEN1基因突变如
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#阿尔茨#
29
#阿尔茨海#
22
赞了,认真探究、学习。
54
非常好的研究,目前阿尔茨海默症的第二条通路研究很少
102
#阿尔茨海默#
27