JAMA Oncol:BMS-986156单药或联合纳武单抗治疗晚期实体肿瘤
2019-11-21 QQY MedSci原创
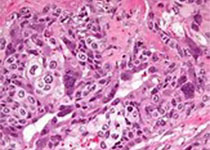
多种免疫刺激激动剂抗体已在实体肿瘤中进行临床试验,以评估靶向糖皮质激素诱导的肿瘤坏死因子(TNF)受体相关蛋白在抗癌治疗中的作用。研究人员开展一全球的、非盲的、1/2a期研究,评估全人糖皮质激素诱导的TNF受体相关蛋白激动剂IgG1单克隆抗体BMS-986156联合或不联合纳武单抗用于晚期实体肿瘤患者的活性和安全性。招募了292位年满18岁的晚期实体瘤患者,ECOG表现状态评分0或1分。单药组:予
研究人员开展一全球的、非盲的、1/2a期研究,评估全人糖皮质激素诱导的TNF受体相关蛋白激动剂IgG1单克隆抗体BMS-986156联合或不联合纳武单抗用于晚期实体肿瘤患者的活性和安全性。招募了292位年满18岁的晚期实体瘤患者,ECOG表现状态评分0或1分。单药组:予以蛋白激动剂BMS-986156,10、30、100、240或800mg/2周,静脉注射;联合组:予以BMS-986156 30、100、240或800mg+纳武单抗 240mg/2周。一个队列还每4周接受480mg BMS-986156和480mg 纳武单抗。主要结点是安全性、耐受性和剂量限制性毒性。次要结点为抗肿瘤活性。
随访了1.4-101.7周(仍在随访中),34位患者(中位年龄56.6岁,16位女性)接受单药治疗(4位完成初始治疗),258位患者(中位年龄60岁,140位女性)接受联合治疗(65位完成了初始治疗)。BMS-986156单药治疗组无3-5级治疗相关副作用事件;联合组有24位(9.3%)患者发生3-4级治疗相关副作用事件,无5级治疗相关副作用。每2周接受800mg BMS-986156+240mg 纳武单抗治疗的患者发生了一例剂量限制性毒性作用;无论是否联合了纳武单抗,BMS-986156在单次给药后均表现出剂量相关性增加的线性的药代动力学。无论是否联合了纳武单抗,BMS-986156注射后外周T细胞和自然杀伤细胞的增殖均增强。未观察到肿瘤内CD8+T细胞和FoxP3+调节性T细胞的一致且显著的调节。仅采用BMS-986156治疗的患者未获得任何缓解;联合组的客观缓解率在0-11.1%,在既往采用抗程序性死亡受体1疗法治疗过的患者中观察到一些缓解。
本研究表明BMS-986156的安全性可控,BMS-986156联合纳武单抗的安全性和疗效可媲美既往纳武单抗单药治疗的相关数据。
原始出处:
Kimberley M. Heinhuis, et al.Safety, Tolerability, and Potential Clinical Activity of a Glucocorticoid-Induced TNF Receptor–Related Protein Agonist Alone or in Combination With Nivolumab for Patients With Advanced Solid Tumors.JAMA Oncol. Published online November 7, 2019.
本文系梅斯医学(MedSci)原创编译,转载需授权!
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#晚期实体肿瘤#
36
#Oncol#
20
#BMS#
30
#实体肿瘤#
41
顶刊就是顶刊,谢谢梅斯带来这么高水平的研究报道,我们科里同事经常看梅斯,分享梅斯上的信息
0
谢谢梅斯分享这么多精彩信息
56