Lancet oncol:口服砒霜+全反式维甲酸或可代替标准三氧化二砷+全反式维甲酸治疗非高风险急性早幼粒细胞白血病!
2018-06-06 MedSci MedSci原创
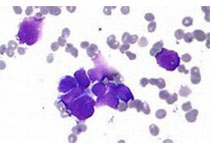
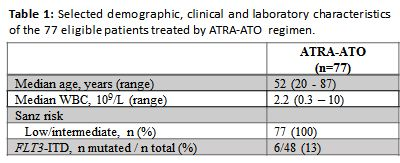
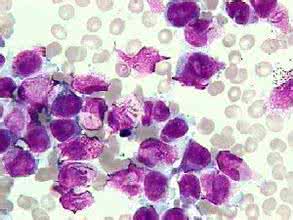
静脉注射三氧化二砷联合全反式维甲酸(ATRA)(无化疗)是非高风险急性早幼粒细胞白血病(白细胞计数≤10x109/L)的标准疗法,可治愈95%以上的病例。但是,一试验性研究,采用口服砒霜(RIF)联合ATRA(无化疗)治疗,比标准静脉疗法更方便,疗效显着。现研究人员对RIF+ATRA与标准静脉三氧化二砷+ATRA疗法治疗非高风险急性早幼粒白血病的效果进行对比。研究人员在中国14个中心进行一非劣效性
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#高风险#
35
#Lancet#
36
#Oncol#
36
#砒霜#
35
#急性早幼粒细胞白血病#
32
#全反式维甲酸#
40
#砷#
30