Chest:社区获得性肺炎住院死亡病例分析!
2018-06-04 xing.T MedSci原创
在这项研究中,在低死亡率的三级护理医院的CAP成年患者,大多数院内死亡似乎没有因住院肺炎护理改善而变得可预防。在护理中存在临终前的限制、高龄和高合并症负担在死亡患者中很是常见。
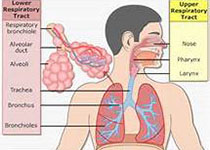
社区获得性肺炎(CAP)住院的成人短期死亡率高。然而,目前尚不清楚医院内肺炎护理的改善能否能大大降低这种风险。近日,呼吸领域权威杂志chest上发表了一篇研究文章,在这项大型前瞻性CAP研究中,研究人员广泛地回顾了所有住院死亡病例,以评估每个死亡患者的原因并评估潜在可预防死亡率的程度。
研究人员在美国五所三级医院招募了住院治疗的CAP患者。五名医生调查员回顾了每一位死亡患者的病历和研究数据库,以确定死亡原因、CAP对死亡的贡献以及任何可能导致死亡的可预防因素。
在2320例招募的患者中,住院期间死亡52例(2.2%)。在这死亡的52例患者中,33例(63.4%)为65岁以上,32例(61.5%)有2种以上的慢性并发症。CAP是27例(51.9%)患者死亡的直接原因。10例(19.2%)患者在入院前没有复苏。4名患者被确定其护理质量的下降可能导致死亡;在这些患者中有两个患者预先存在的生命终结疾病。两名寻求全面医疗护理的患者经历了医院内的肺炎护理质量的下降,可能促进其死亡。
在这项研究中,在低死亡率的三级护理医院的CAP成年患者,大多数院内死亡似乎没有因住院肺炎护理改善而变得可预防。在护理中存在临终前的限制、高龄和高合并症负担在死亡患者中很是常见。
原始出处:
Grant W. Waterer,et al. In-hospital Deaths among Adults with Community-Acquired Pneumonia.chest.2018. https://doi.org/10.1016/j.chest.2018.05.021
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#EST#
32
#死亡病例#
23
#获得性#
34
#Chest#
24
#社区#
30
学习了.谢谢分享.
48
学习了受益匪浅
38