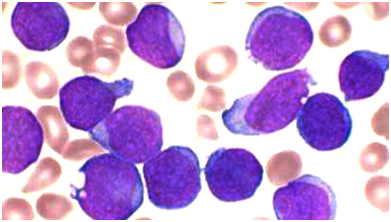
Blood:MELK-EZH2泛素化或可成为NKTL的治疗新靶点
2019-08-25 MedSci MedSci原创
癌原性EZH2在包括结外自然杀伤细胞/T细胞淋巴瘤(NKTL)在内的各种癌症中过表达,广泛参与其病理生理过程。但是,EZH2表达上调的机制尚不明确。在本研究中,Boheng Li等研究人员检测了NKTL中EZH2蛋白的转化率,发现MELK激酶是EZH2泛素化和转化率的调节因子。采用质谱定量分析(MS),研究人员观察到MELK介导的EZH2 S220磷酸化增加,同时伴有EZH2 K222泛素化缺失,
癌原性EZH2在包括结外自然杀伤细胞/T细胞淋巴瘤(NKTL)在内的各种癌症中过表达,广泛参与其病理生理过程。但是,EZH2表达上调的机制尚不明确。
在本研究中,Boheng Li等研究人员检测了NKTL中EZH2蛋白的转化率,发现MELK激酶是EZH2泛素化和转化率的调节因子。采用质谱定量分析(MS),研究人员观察到MELK介导的EZH2 S220磷酸化增加,同时伴有EZH2 K222泛素化缺失,提示EZH2泛素化受磷酸化依赖性调控。
通过化学和遗传途径抑制MELK导致EZH2蛋白泛素化和去稳定化。此外,研究人员还发现MELK在NKTL中表达上调,其表达与NKTL患者组织芯片检测的EZH2蛋白表达相关。但在胶质瘤中,连接MELKEZH2信号的FOXM1并没有参与介导EZH2泛素化。此外,研究人员还明确了USP36是一个去泛素化酶,可催化EZH2 K222位点去泛素化。
本研究揭示了MELK和USP36在NKTL中介导EZH2稳定性方面的重要作用。MELK过表达通过抑制EZH2泛素化降低NKTL对硼替佐米治疗的敏感性。因此,靶向MELK调控EZH2泛素化状态可能是对硼替佐米治疗反应不良的NKTL患者的一种新的治疗策略。
原始出处:
Boheng Li,et al.MELK mediates the stability of EZH2 through site-specific phosphorylation in extranodal natural killer/T-cell lymphoma.Blood 2019 :blood.2019000381; doi: https://doi.org/10.1182/blood.2019000381
本文系梅斯医学(MedSci)原创编译,转载需授权!
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#NKT#
38
#Ezh2#
24
#新靶点#
20
#治疗新靶点#
30
好
60