Int J Dev Neurosci:感觉神经性听力损失患者的左枕外侧皮质厚度减少
2019-06-16 AlexYang MedSci原创
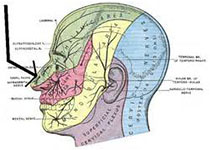
感觉神经性听力损失患者(SNHL)倾向于表现出语言发育延迟、执行功能缺陷和视觉认知障碍,甚至是听力扩大和耳蜗移植介入之后,仍旧表现出上述情况,表明了SNHL患者中大脑结构和功能已经发生了改变。最近,有研究人员调查了30名SNHL儿童中大脑MRI结构情况(18名轻度到中度SNHL(M-M),12名重度到永久性SNHL(M-P)),并与性别和年龄相匹配的正常对照(NC)进行了比较。研究发现,区域分析表
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#感觉神经#
38
#神经性#
34
#听力#
31
#ROS#
40
#Dev#
33