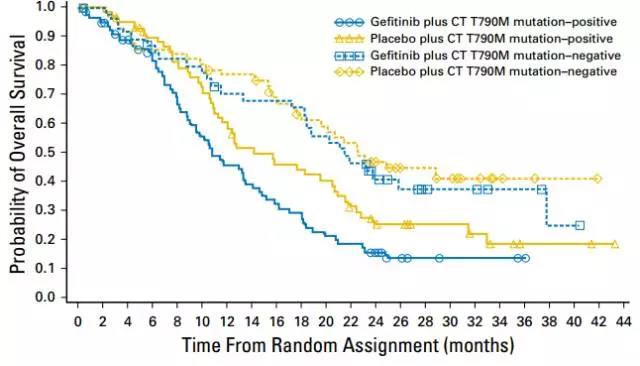
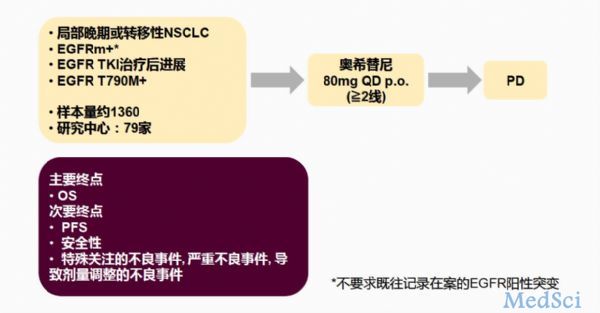
JCO:IMPRESS研究公布最终OS结果:耐药后EGFR –TKI原药能不能继续使用?
2017-10-12 wrangx “肿瘤资讯”微信号
EGFR突变阳性晚期NSCLC一代EGFR-TKI继发耐药后,化疗联合EGFR-TKI原药使OS受损,通过IMPRESS研究Tony Mok教授警示大家,一代EGFR-TKI耐药后如果选择化疗不要再联合原来使用EGFR-TKI药物。

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#IMPRESS研究#
32
#JCO#
35
学习了.获益匪浅!感谢分享
49
不错的.学习了!谢谢分享!
49
非常好.学习了.很受益
56
#TKI#
22
#GFR#
28