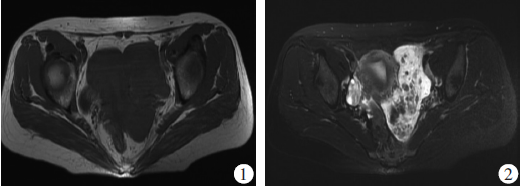
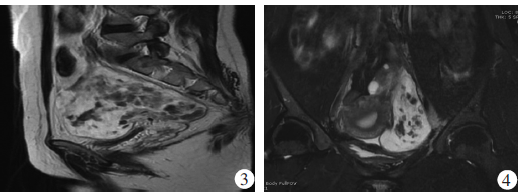
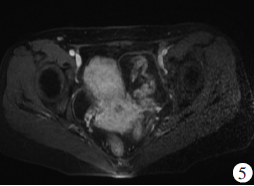
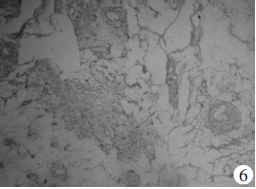
原发性盆腔腹膜后平滑肌瘤误诊为卵巢囊腺瘤一例
2019-02-25 徐树明 李素红 实用医学影像杂志
患者女,38岁,主诉:发现“盆腔肿物”1年余;现病史:2014年7月体检彩色多普勒超声发现:左附件区肿物,大小约6.0 cm×6.0 cm,无腹痛、腹胀,无发热、无月经改变,未正规治疗。于2015年2月15日就诊于我院行彩色多普勒超声提示:左附件区探及7.3 cm×6.8 cm×5.0 cm低回声不均质肿物,测CA125为12.1U/mL,建议住院治疗,患者拒绝,予以口服红金消结片、桂枝茯苓胶囊1
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#腹膜后#
27
#平滑肌#
23
#卵巢囊#
30
#原发性#
27
#平滑肌瘤#
34
#腹膜#
29