Neurology:血管内取栓术后罕见并发症1例
2018-02-14 杨中华 脑血管病及重症文献导读
46岁,女性,因严重左侧半球综合征到急诊室就诊,NIHSS 11分。
46岁,女性,因严重左侧半球综合征到急诊室就诊,NIHSS 11分。
下图,DSA显示左侧MCA血栓(A图),血栓切除术后完全再通(B图)。随访DWI显示左侧MCA分布区小片梗死(C图):

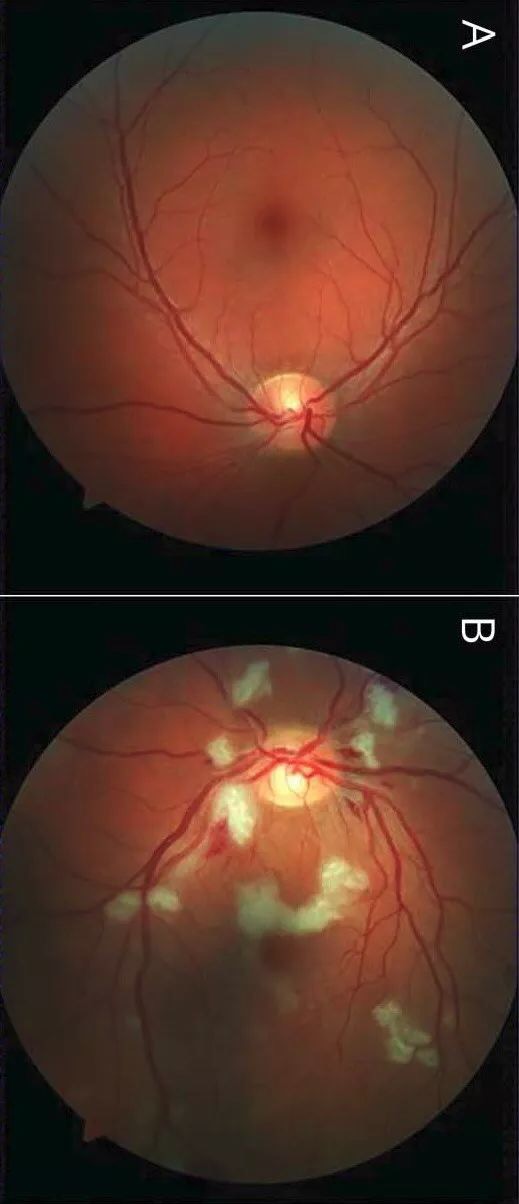
眼底镜检查显示左眼视网膜缺血,未见血管闭塞(下图)。推测可能由于短暂血栓栓塞所致,作者认为这是血栓切除术罕见的并发症。
下图,眼底镜检查。右眼未见明显异常(A图);左眼显示视网膜出血,以及棉絮状渗出(视网膜缺血的征象):
原始出处:
Manuel Bolognese, et al. Teaching NeuroImages: Visual loss as a rare complication of mechanical thrombectomy. Neurology.2018 Jan 23;90(4):e355-e356.doi:10.1212/WNL.0000000000004863.
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#Neurol#
33
#取栓术#
50
#并发#
29
认真学习天天向上
54
#罕见#
31
#取栓#
41