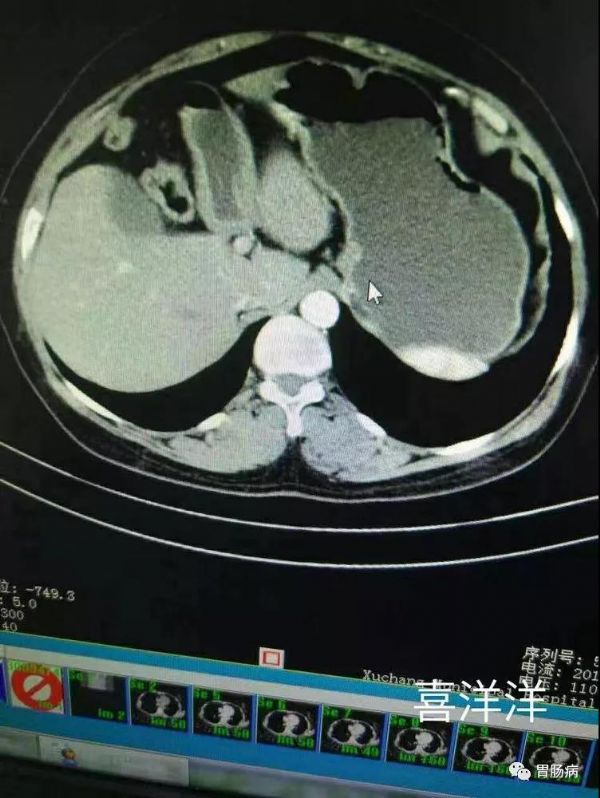
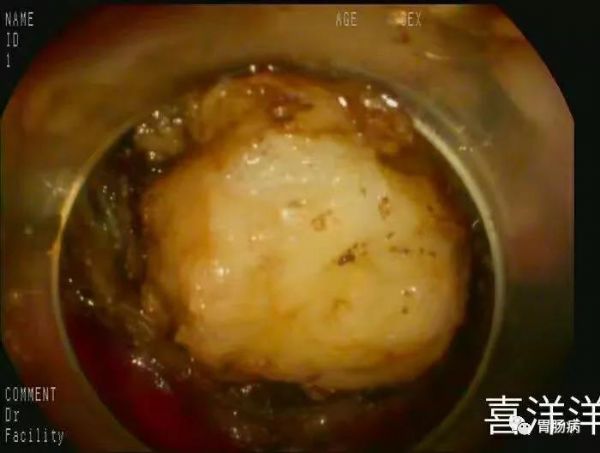
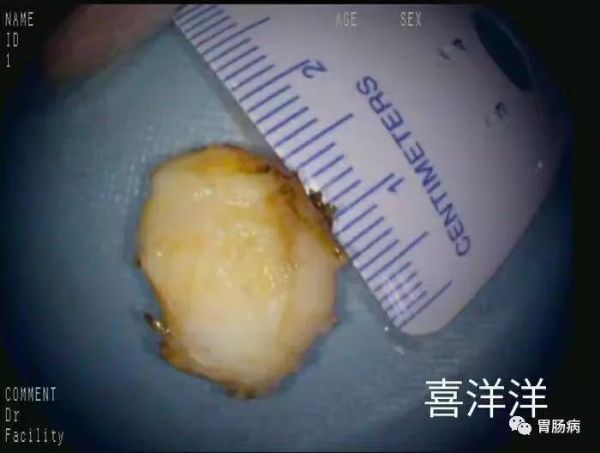
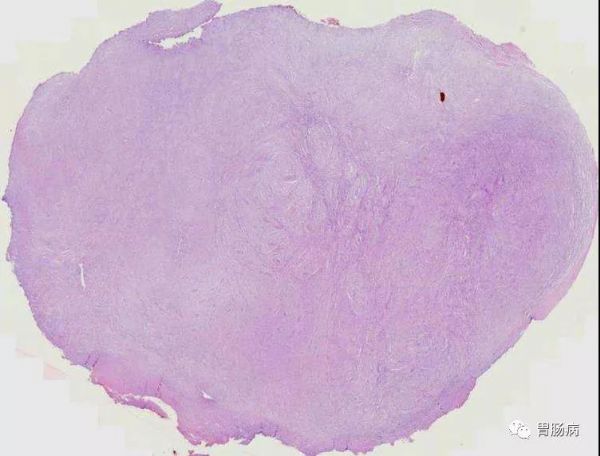
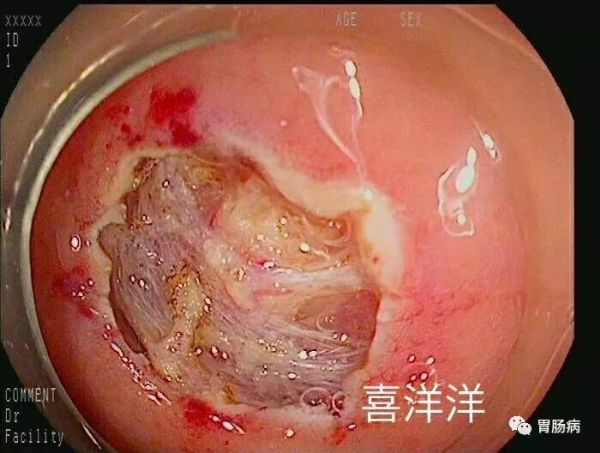
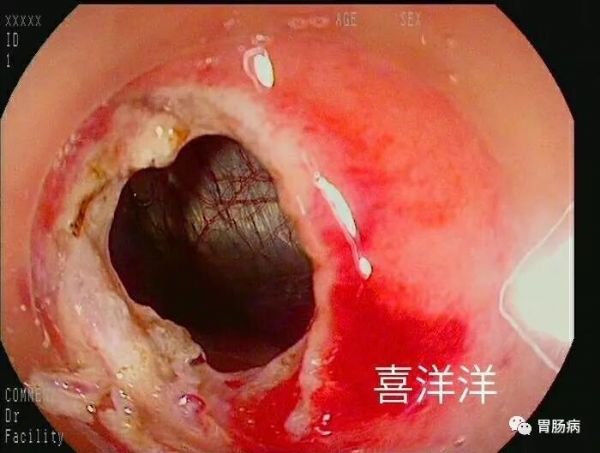
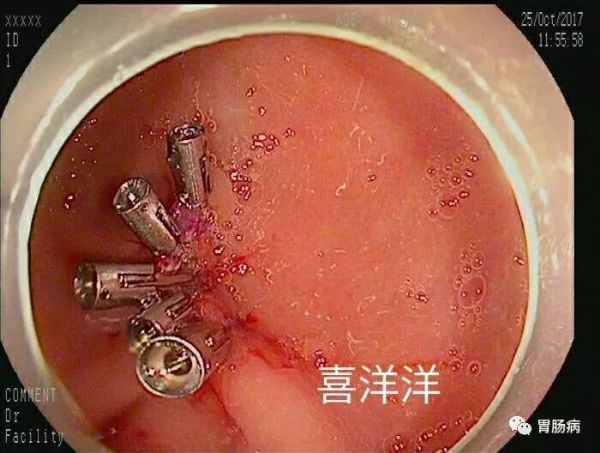
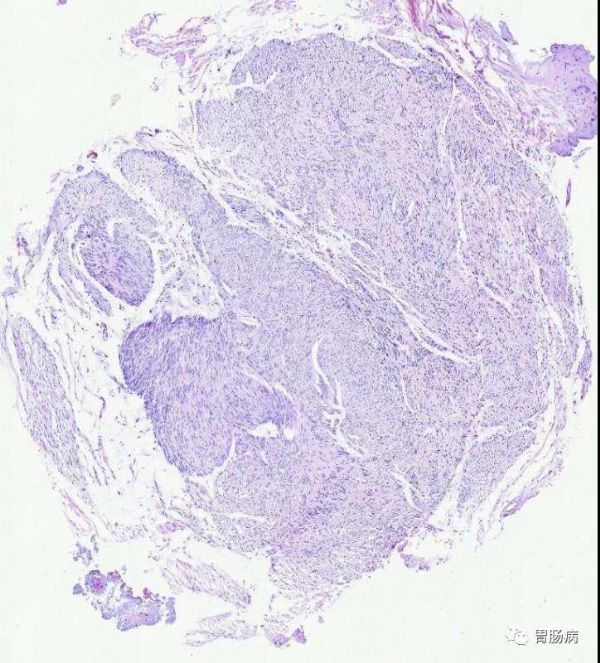
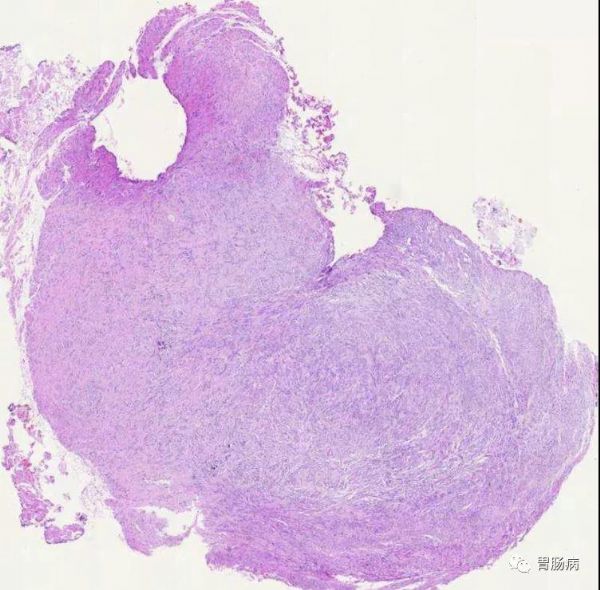
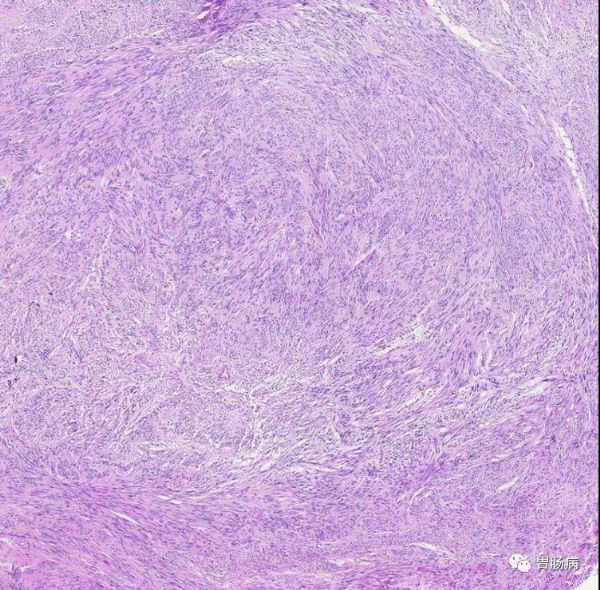
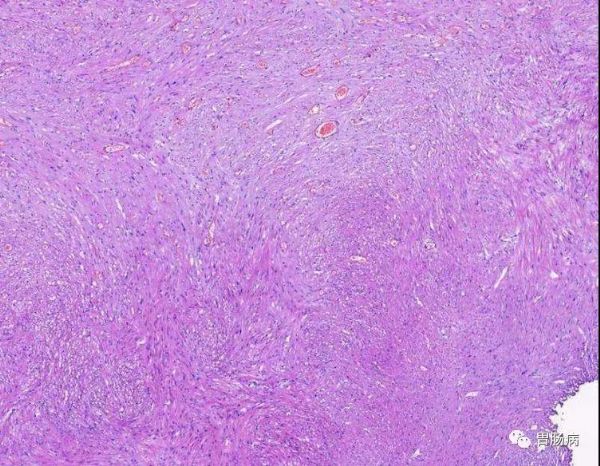
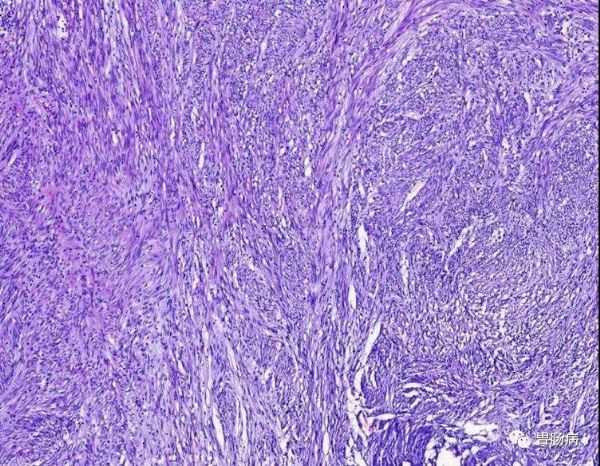
形形色色的胃肠道间质瘤,内镜下该如何破?(实战篇)
2019-11-12 杨喜洋 胃肠病
“医贵乎精,学贵乎博,识贵乎卓,心贵乎虚,业贵乎专,言贵乎显,法贵乎活,方贵乎纯,治贵乎巧,效贵乎捷。知此乎,则医之能事毕矣。”
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言


































文案不错!
75
非常受益,很好的研究
96
非常受益,很好的研究
84
非常受益,很好的研究
88
#内镜#
46
#胃肠道#
39
#间质瘤#
29