日本推出慢性心衰新药——Coralan(伊伐布雷定)
2019-12-02 生物谷 生物谷
日本药企小野制药(Ono Pharmaceutical)近日宣布,推出心衰药物Coralan(通用名:ivabradine hydrochloride,盐酸伊伐布雷定)2.5mg、5mg、7.5mg。该药是一种超极化激活环核苷酸门控(HCN)通道抑制剂,于今年9月获得批准,用于治疗窦性心律中静息心率≥75次/分钟的慢性心力衰竭(CHF)患者(仅限于正接受标准治疗的CHF患者,包括β-受体阻滞剂)。
日本药企小野制药(Ono Pharmaceutical)近日宣布,推出心衰药物Coralan(通用名:ivabradine hydrochloride,盐酸伊伐布雷定)2.5mg、5mg、7.5mg。该药是一种超极化激活环核苷酸门控(HCN)通道抑制剂,于今年9月获得批准,用于治疗窦性心律中静息心率≥75次/分钟的慢性心力衰竭(CHF)患者(仅限于正接受标准治疗的CHF患者,包括β-受体阻滞剂)。
Coralan的批准,主要基于2项临床研究的数据:(1)一项多中心、随机、双盲、安慰剂对照研究(J-SHIFT),在日本245例慢性心力衰竭患者(纽约心脏协会[NYHA]心功能分级II-IV级,窦性心律中静息心率≥75次/分钟,接受最佳背景疗法的情况下左心室射血分数[LVEF]≤35%)中开展;(2)一项多中心、随机、双盲、安慰剂对照研究(SHIFT),在海外6505例慢性心力衰竭患者(窦性心律中静息心率≥70次/分钟)中开展,该研究与J-SHIFT研究类似。
心力衰竭(HF)是指由于心功能障碍导致心泵代偿功能衰竭而出现呼吸困难、疲劳和水肿,导致运动耐力下降的一种临床综合征。慢性心力衰竭(CHF)是HF的慢性持续状态。在日本,据估计2020年CHF患者将达到120万。治疗CHF的药物包括血管紧张素转换酶抑制剂、血管紧张素受体拮抗剂、β受体阻滞剂、抗醛固酮药物、利尿剂等,目的是控制CHF患者的症状,预防CHF患者住院、避免死亡。
在CHF患者中,心率趋于增加,以补偿心脏无法发挥泵出足够的血容量,从而使心脏承受更大的压力。此外,高心率对CHF患者的预后也有负面影响。Coralan将为高心率患者提供一种新的治疗选择,即使他们正在服用现有药物治疗CHF。
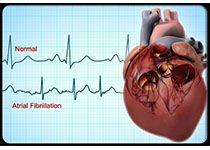
Coralan的活性药物成分为ivabradine,这是全球首个选择性特异性If电流抑制剂——心脏激动剂,具有特殊的降低心率作用,选择性作用于窦房结,自发舒张去极化并调节心率,而对心内传导、心肌收缩力或心室复极化无影响。
ivabradine由法国制药公司施维雅(Servier)发现和开发,在欧盟分别于2005年10月和2012年2月获批,用于慢性稳定型心绞痛和慢性心力衰竭的治疗。截至目前,ivabradine已获全球120多个国家和地区批准,其中110多个国家批准用于慢性稳定型心绞痛和慢性心力衰竭适应症。
根据2011年9月与施维雅签订的许可协议,小野制药拥有在日本的开发和商业化ivabradine治疗慢性心力衰竭(CHF)的独家权利。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#Oral#
46
#ALA#
28
#日本#
31
#伊伐布雷定#
38