AJG:CK18或可成为无创诊断儿童非酒精性脂肪性肝炎的标志物
2013-09-27 tiancai_erbao DXY
研究热点: 1.本研究的目的在于评估检测血清中细胞角蛋白-18(CK18)片段水平作为无创性诊断小儿非酒精性脂肪性肝炎的有效标志物的可行性。 2.经肝组织活检确诊为非酒精性脂肪性肝炎的患儿同时抽取血液样本,采用凋亡敏感酶联免疫吸附试验试剂盒测定血清中CK18的水平。 3.血清CK18在非酒精性脂肪性肝炎患儿中明显升高,具有良好的敏感性和特异性。血清CK18每升高10U/L,则发生非酒精性脂肪
研究热点:
1.本研究的目的在于评估检测血清中细胞角蛋白-18(CK18)片段水平作为无创性诊断小儿非酒精性脂肪性肝炎的有效标志物的可行性。
2.经肝组织活检确诊为非酒精性脂肪性肝炎的患儿同时抽取血液样本,采用凋亡敏感酶联免疫吸附试验试剂盒测定血清中CK18的水平。
3.血清CK18在非酒精性脂肪性肝炎患儿中明显升高,具有良好的敏感性和特异性。血清CK18每升高10U/L,则发生非酒精性脂肪性肝炎的可能性增加大约70%。
非酒精性脂肪性肝炎是非酒精性脂肪性肝病中进展最为迅速的一类。在儿童中,寻找一种无创性诊断非酒精性脂肪性肝炎的方法迫在眉睫。当肝细胞发生凋亡时,血清中细胞角蛋白-18片段水平会增加,并作为衡量肝细胞凋亡水平的标志物。美国加州加州大学圣地亚哥分校雷迪儿童医院儿科胃肠病、肝病及营养科的Ariel E. Feldstein等人对检测血清中细胞角蛋白-18(CK18)片段水平能否作为无创性诊断小儿非酒精性脂肪性肝炎的有效标志物的可行性进行了评估。【原文下载】
将连续获得活检诊断证实为非酒精性脂肪性肝病的患儿为研究对象。收集进行活检时的血液样本。非酒精性脂肪性肝病的诊断依据布鲁特标准。组织学特征按照下列病变评分:脂肪变性(0-3)、小叶炎症(0-3)、气球样变(0-2)、汇管区炎症(0-2)。计算非酒精性脂肪性肝病活动度评分(0-8)以及纤维化程度评分(0-4)。我们使用M-30凋亡敏感酶联免疫吸附试验试剂盒测定血清中CK18的水平。
共有201名实验对象纳入研究。平均年龄10.7±2.5岁。37%为男性。其中140名患者诊断为非酒精性脂肪性肝炎,平均非酒精性脂肪性肝病活动评分为4.4±1.3。其中非酒精性脂肪性肝炎患儿的血清CK18水平显著高于并非非酒精性脂肪性肝炎的患儿(322.1 U/l±104.8 vs. 164.2 U/l±62,P<0.001)。在活检中诊断非酒精性脂肪性肝炎的风险升高与血清中CK18升高的水平相一致 (P<0.001)。在排除校正各种混杂因素后,血清CK18每升高10U/L,则发生非酒精性脂肪性肝炎的可能性增加大约70%。血清CK18水平用于诊断非酒精性脂肪性肝炎的性能是十分优异的。其接受者操作特征曲线下面积为0.933。
由此可见,CK18有望成为脂肪性肝病儿童中诊断非酒精性脂肪性肝炎的无创性标志物。
研究背景:
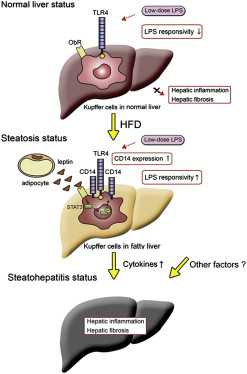
儿童非酒精性脂肪性肝病是一组包含有多种组织学改变的疾病谱。包括有以甘油三酯为主的脂肪在肝细胞内聚集的孤立性肝脂肪变、以脂质堆积伴随肝细胞受损、炎症细胞浸润为主要特征的非酒精性脂肪性肝炎以及不同程度的肝纤维化等等。非酒精性脂肪性肝炎是其中较为严重的一种,可逐渐演变为肝硬化,并且在儿童期即可出现一系列严重并发症。
目前诊断非酒精性脂肪性肝炎的金标准是肝组织活检。然而因该检查方法为有创性、价格较贵、又有出血、感染等并发症发生的风险,所以难以在儿童患者诊断中的应用受到了很大限制。且非酒精性脂肪性肝炎的患儿多数无明显症状,肝组织活检很难起到筛查以及监测的作用。因此寻找高敏感性与特异性的筛查替代方法尤为重要。
血清细胞角蛋白-18是肝脏中间丝蛋白。当受到脂肪堆积影响而受损的肝细胞发生凋亡时,细胞凋亡蛋白酶裂解的CK-18片段被释放入血液,导致血清中CK18水平升高。因这种肝细胞凋亡的激活为非酒精性脂肪性肝炎所特有,而在肝细胞脂肪变性中并不存在,所以血清中CK-18的水平可以用来鉴别这两种疾病。在成人中,已有相关研究表明,CK18可以作为鉴别成人非酒精性脂肪性肝炎和肝细胞脂肪变性的标志物。一项多中心研究也证实,在成人中,血清CK18水平每升高50U/L,则经肝组织活检确诊为非酒精性脂肪性肝炎的几率上升30%。因检测血清CK18仅需要抽取血液样本,所以这种方法对儿童很适用。
基于上述研究背景,本实验的研究目的即为在一个经肝组织活检证实的、良好分组的非酒精性脂肪性肝病儿童患者的大样本人群中研究血清CK18水平可否作为儿童非酒精性脂肪性肝炎的诊断标志物。
原文下载
Feldstein AE, Alkhouri N, De Vito R, Alisi A, Lopez R, Nobili V.Serum cytokeratin-18 fragment levels are useful biomarkers for nonalcoholic steatohepatitis in children.Am J Gastroenterol. 2013 Sep;108(9):1526-31.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#AJG#
27
#无创诊断#
33
#脂肪性肝炎#
24
#标志物#
27
#酒精性#
31
#非酒精性#
32
#脂肪性#
46