JAMA Neurol:卒中慢性期症状复发,DWI无新发病灶怎么回事?
2017-10-08 杨中华 脑血管病及重症文献导读
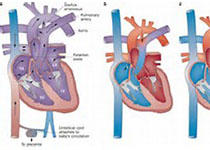
相信大家都见过类似的病例: 女性,50s。既往慢性高血压、糖尿病。7年前隐源性脑卒中,当时NIHSS评分12分,左侧面、上肢和下肢无力,左侧感觉丧失,3个月后症状完全恢复。

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#Neurol#
35
学习一下
75
学习
64
hhhhhe
66
#DWI#
37
学习
83
学习了新知识
58
学习一下知识
30
受益匪浅.精彩的內容
26
卒中慢性期神经系统缺损短暂恶化.或先前卒中相关缺损再次出现(或脑卒中后症状重现.poststrokerecrudescence.PSR)是一种常碰到的现象.
0