Stroke:可识别症状性颅内出血高风险卒中患者的新工具!
2018-02-11 贾朝娟 环球医学
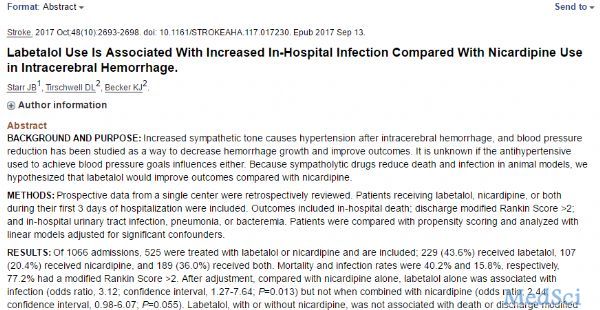
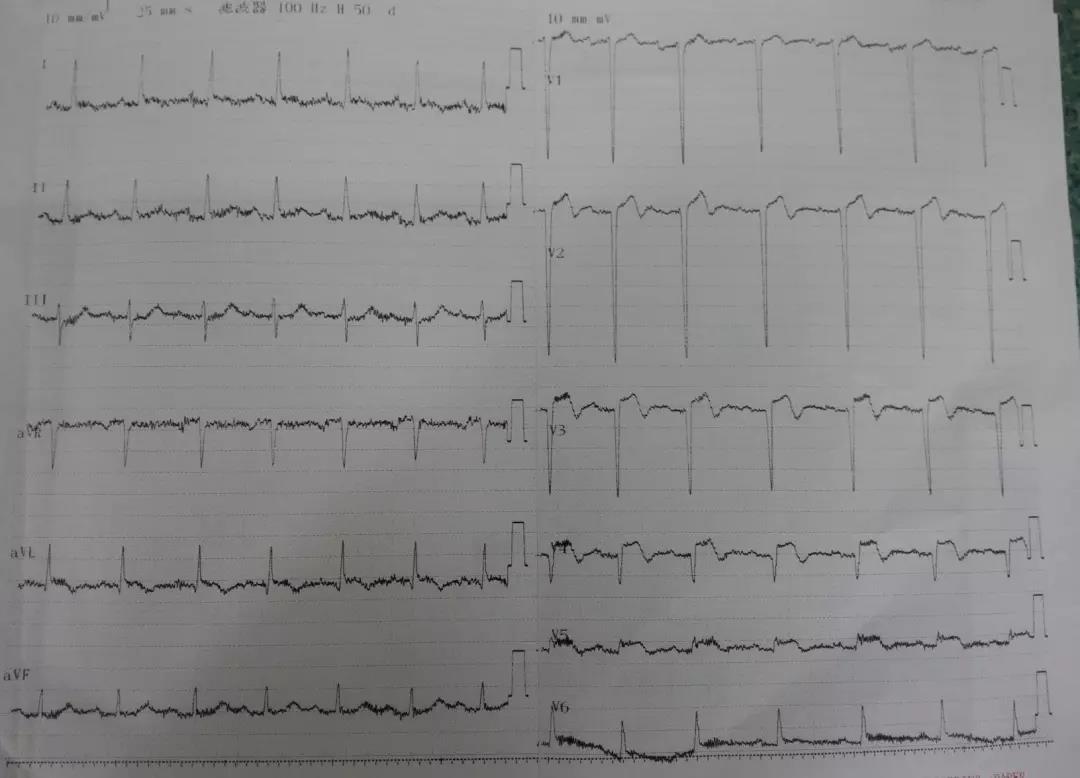
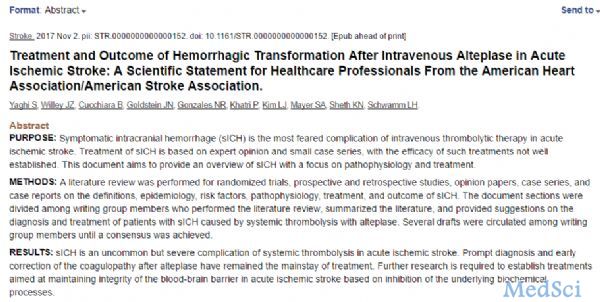
静脉溶栓可以挽救卒中患者的生命,但使用不当也可以给患者带来新的伤害,如症状性颅内出血(sICH)。如何准确识别适合进行静脉溶栓的卒中患者,是治疗发挥最大获益避免伤害的关键。2018年2月,发表子《Stroke》的一项研究为大家绘制出了可以个体化预测静脉溶栓治疗卒中患者sICH风险的列线图。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#高风险#
27
好好学习认真听讲为人民服务
48
#卒中患者#
32
好好学习学习
45
优质资源.共同学习
61