Ann Rheum Dis:精氨酸酶II在骨关节炎发病机制中的关键作用
2019-01-05 xiangting MedSci原创
这项研究结果表明Arg-II是小鼠OA发病机制的关键调节因子。
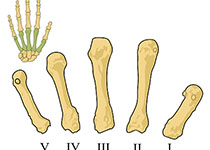
骨关节炎(OA)似乎与各种代谢紊乱有关,但氨基酸代谢对OA发病机制的潜在影响尚未被明确阐述。这项研究探讨了软骨细胞氨基酸代谢的改变是否可以调节OA发病机制。
通过微阵列分析检测原代培养传代0小鼠软骨细胞中氨基酸代谢调节基因的表达谱,并在小鼠OA软骨细胞和人、小鼠模型的OA软骨中进一步表征所选基因。通过内侧半月板去稳定化(DMM)或关节内(IA)注射表达分解代谢调节剂的腺病毒诱导小鼠实验性OA。在Arg2-/- 小鼠和IA注射编码Arg-II腺病毒(Ad-Arg-II)的小鼠中检测精氨酸酶II(Arg-II)的功能结果。
在各种病理情况下及人类OA患者和各种小鼠模型的OA软骨中,软骨细胞中编码精氨酸代谢酶Arg-II的基因均特异性上调。小鼠关节组织中腺病毒介导的Arg-II过表达引起OA发病,而小鼠中Arg2的基因切除(Arg2-/-)消除了DMM诱导OA的所有表现。从机制上讲,Arg-II似乎至少部分通过核因子(NF)-κB途径上调软骨细胞中基质降解酶(基质金属蛋白酶3[MMP3]和MMP13)的表达而导致OA的软骨破坏。
这项研究结果表明Arg-II是小鼠OA发病机制的关键调节因子。虽然人类和小鼠的软骨细胞并不相同,但同样对Arg-II有反应,研究结果表明Arg-II可能是OA发病机制的治疗靶点。
原始出处:
Wan-Su Choi. Critical role for arginase II in osteoarthritis pathogenesis. Ann Rheum Dis. 04 January 2019.
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#精氨酸#
33
#中的关键作用#
27
#精氨酸酶II#
27
#Dis#
25
#骨关节#
30
#关节炎#
34