Nature:上海中科院药物所新成果促进糖尿病新药开发
2018-01-04 黄辛 中国科学报
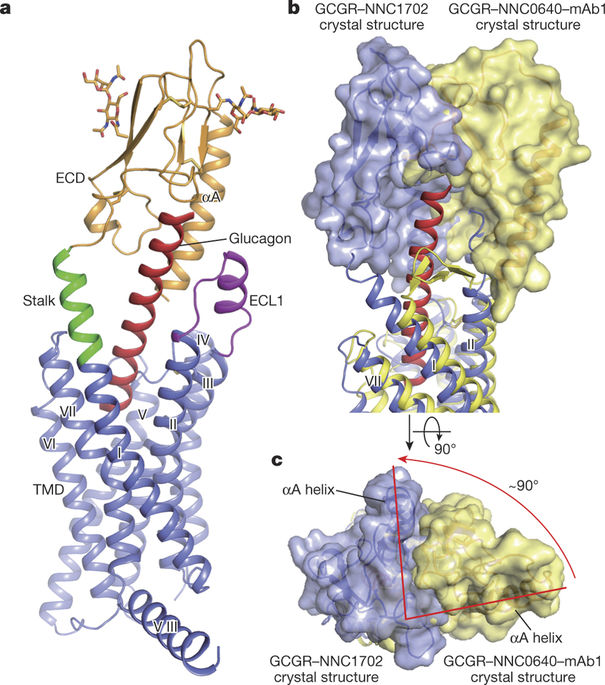
中科院上海药物研究所吴蓓丽课题组和赵强课题组在B型G蛋白偶联受体(GPCR)结构与功能研究领域又获重要突破,首次测定了胰高血糖素受体(GCGR)全长蛋白与多肽配体复合物的三维结构,揭示了该受体对细胞信号分子的特异性识别及其活化调控机制。该成果1月4日发表于《自然》杂志。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#Nat#
32
#新成果#
0
#新药开发#
35
#中科院#
22
henhao
67