名家观点系列(三):SECURE-PCI及相关研究解读与启示
2018-05-16 国际循环编辑部 国际循环
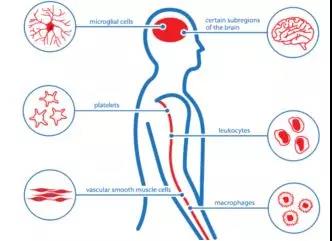
急性冠状动脉综合征(Acute Coronary Syndrome,ACS)病情非常凶险,临床上以发作急、病情重和致死率高为特点。规范ACS的诊疗对于降低其死亡率和再发生率具有重要的价值。国内外ACS相关指南均强调强化他汀治疗在ACS治疗中的一线地位(IA)。近日,美国心脏病学会(American College of Cardiology,ACC)年会上发布的SECURE-PCI研究表明,对于A
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言




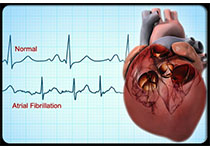






#SECURE-PCI#
40
#Cure#
25
急性冠状动脉综合征相关研究.
71
急性冠状动脉综合征相关研究.
83
#相关研究#
26
急性冠状动脉综合征相关研究.
0
急性冠状动脉综合征相关研究.
59