Diabetes Care:严重低血糖与2型糖尿病成人心血管事件和死亡率之间的相关性分析!
2017-11-11 xing.T MedSci原创
由此可见,严重低血糖可表明患者健康状况下降,是较高的心血管事件和死亡率绝对风险强有力的标志。
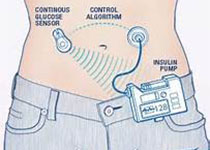
有证据表明低血糖与心血管疾病有关,但在社区为基础的研究中收集的数据很少。个别心血管结局和疾病特异性死亡率的信息缺乏。近日,糖尿病领域权威杂志Diabetes Care上发表了研究文章,研究人员对来自于社区动脉粥样硬化风险研究(ARIC)(分析的基线为1996-1998年)的1209名被诊断为糖尿病参与者进行了一项前瞻性队列分析。
严重低血糖发作是通过直至2013年期间的住院、急救科就诊和救护电话中首次的ICD-9编码来进行确定,并且确定了心血管事件和死亡情况。研究人员使用调整后的采用低血糖作为随时间变化的暴露Cox回归模型进行分析。
研究人员发现在中位数为15.3年的随访期间195名参与者至少发生过一次严重低血糖事件。严重低血糖后,冠心病的3年累计发病率为10.8%,病死率为28.3%。调整后,严重低血糖与冠心病(风险比为2.02,95%可信区间为1.27-3.20)、全因死亡率(风险比为1.73,95%可信区间为1.38-2.17)、心血管死亡率(风险比为1.64,95%可信区间为1.15-2.34)和癌症死亡率(风险比为2.49,95%可信区间为1.46-4.24)有关。低血糖与脑卒中、心力衰竭、心房颤动或非心血管和非癌症死亡无关。这些结果在年龄、性别、种族、糖尿病病程和基线心血管风险方面定义明确的亚组中较为明显。
由此可见,严重低血糖可表明患者健康状况下降,是较高的心血管事件和死亡率绝对风险强有力的标志。
原始出处:
Alexandra K. Lee, et al. The Association of Severe Hypoglycemia With Incident Cardiovascular Events and Mortality in Adults With Type 2 Diabetes.Diabetes Care 2017. https://doi.org/10.2337/dc17-1669
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#血管事件#
36
#相关性#
29
#BET#
40
#严重低血糖#
37
#Diabetes#
31
#DIA#
36
好好看下.内容丰富
65
讲解的非常好,值得学习
73
#相关性分析#
39
学习了.谢谢.
68