2018年ICRNM现场精彩呈现:低蛋白饮食对CKD患者的肾功能具有保护作用
2018-07-02 MedSci MedSci原创
2018年6月26日至30日,第19届国际肾脏营养与代谢学会大会(ICRNM)在意大利热那亚举行,在此,我们将第一时间为您翔实介绍会议上提出的最新观点与最新进展。
国际肾脏营养与代谢学会(ISRNM)是重要的肾脏科学组织,致力于肾脏疾病的营养和新陈代谢的研究与教育。ISRNM通过每年两次的多学科国际大会、肾脏营养学报和科学声明将科学家、公共卫生官员、执业医师和营养师紧密联系在一起,第一时间分享肾病领域的最新临床和科学信息。2018年6月26日至30日,第19届国际肾脏营养与代谢学会大会(ICRNM)在意大利热那亚举行,在此,我们将第一时间为您翔实介绍会议上提出的最新观点与最新进展。
专家简介
Liliana Garneata,罗马尼亚卡罗尔达维拉医学和药学大学教授,肾病领域专家,经谷歌学术统计,Liliana Garneata教授文章引用次数高达1029次,h-Index为18。

背景简介--CKD的威胁
随着人口老龄化,可引起肾脏损伤的高血压、糖尿病等疾病的发病率正在逐年增加,因此慢性肾病(chronic kidney disease,CKD)已经成为威胁全世界公共健康的主要疾病,CKD不仅发病率高、致死率高,而且可以引起心、脑等多器官损害。发达国家的CKD发病率为6.5-16%,我国的CKD发病率大于10%。CKD是由各种原因引起的,对健康有影响的肾脏结构或功能异常大于3个月,包括肾小球滤过率(GFR)下降或肾脏损伤标志物异常,如组织学、影像学检查异常、白蛋白尿等异常。若肾脏疾病(如肾小球肾炎、IgA肾病、隐匿性肾炎、膜性肾病、肾盂肾炎、过敏性紫癜肾炎、痛风肾、红斑狼疮肾炎、肾病综合征、糖尿病肾病、高血压肾病)病程超过3个月,可统称为CKD。
近年来,大量研究表明,合理调整CKD患者的饮食结构对患者疾病的改善尤为重要,这里我们将重点介绍低蛋白饮食对CKD患者的影响。
什么是低蛋白饮食(LPD)?
低蛋白饮食(LPD)是指限制日常饮食中的蛋白质供摄入,大量临床研究表明,LPD不仅能降低甘油三酯、胆固醇水平,改善血脂代谢,减少蛋白质分解代谢物的生成和蓄积,减少CKD患者的蛋白尿水平,而且能通过降低肾小球的高灌注及高滤过来保护肾单位,进而减轻残余肾单位高负荷的工作状态,达到延缓肾小球的硬化和疾病进展的目的。反之,高蛋白饮食加重肾脏高滤过状态,患者尿蛋白、尿素、肌酐等指标将持续恶化。
正常人最低蛋白推荐摄入量(RDA)一般在每天每公斤体重摄入0.8克蛋白质左右,这里值得注意的是,低蛋白饮食的错误使用容易导致过低的蛋白摄人,造成必需氨基酸的缺乏,因此对低蛋白饮食配方的改善就显得尤其关键,这就涉及了LPD、sVLPD及KA的概念。除此之外,LPD还面临着患者认知不足、依从性较差等诸多困难。
在我们开始详细介绍LPD之前,我们依然要明晰几个概念,即NPD、LDP及sVLDP。NPD:normal-protein diet正常蛋白饮食;LPD:low-protein diet 低蛋白饮食,0.6-0.8 g/kg每天;sVLPD:supplemented very low protein diet,0.3-0.4 g/kg每天,同时补充必需氨基酸及酮酸(Ketoacids ,KAs)。
CKD患者如何获益于LPD?
LPD降低蛋白尿及磷酸盐水平
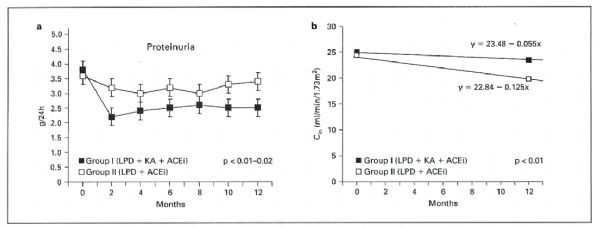
我们知道,在LPD中补充酮酸类似物有助于蛋白质的代谢,那么补充有酮酸类似物的LPD是否能改善患者的病理状态呢?答案是肯定的,如图所示,在0-12个月内,补充酮酸类似物的LPD组患者的蛋白尿水平始终显着低于LPD组[1]。
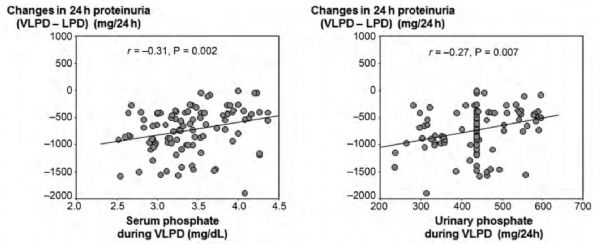
酮酸类似物补充剂不仅对尿蛋白有影响,在矿物质代谢方面也有改善作用。CKD终末期患者常合并高磷血症,那么高磷血症患者能否从补充KA中获益呢?近期的研究表明,相比于LPD,VLPD(含有酮酸类似物补充剂)组患者的蛋白尿水平显着降低,血液磷酸盐水平显着下降[2]。
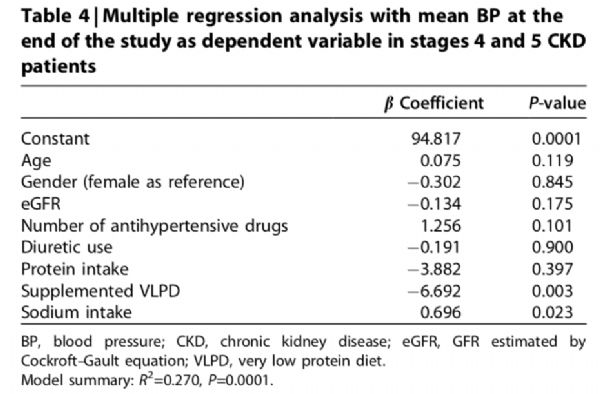
sVLPD改善了血压控制
在CKD治疗中,患者血压(BP)通常难以控制,那么LPD与sVLPD是否能改善CKD患者的血压控制呢?一项前瞻性研究招募了110例4-5期的CKD患者,对比了LPD与sVLPD在血压控制方面的差异,结果表明,在sVLPD组中,BP显着降低,且BP、尿钠排泄与酮酸类似物独立相关[3]。
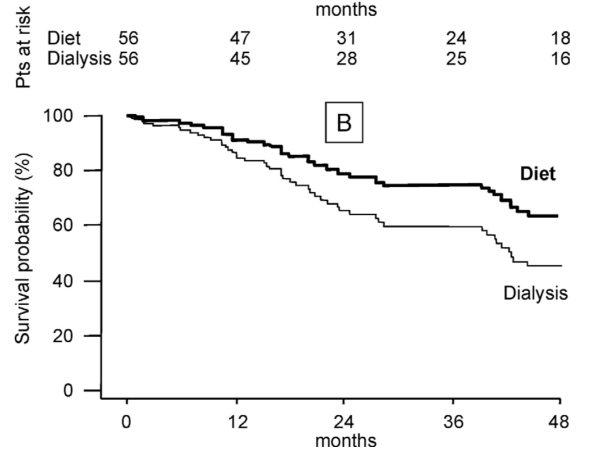
sVLPD推迟透析
终末期肾病(ESRD)是慢性肾病(CKD)的最后阶段(CKD 5期),当CKD进展至 ESRD时,需要肾脏替代治疗(RRT),RRT包括透析(血液透析或腹膜透析)和肾脏移植。那么LPD与sVLPD是否能延缓CKD患者进入透析呢?一项随机对照试验分析了56例非糖尿病老年CKD患者,发现sVLPD将RRT的启动延迟了约1年,且不会增加其死亡或住院风险[4]。
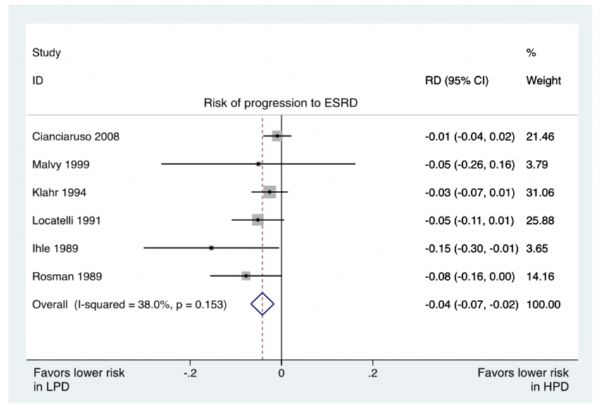
另外,一项荟萃分析研究验证了LPD对CKD的治疗是安全有效的,能够延迟透析而不引起蛋白质能量消耗或恶病质,具体结果表明,LPD将CKD进展至ESRD风险降低了4%[5]。
总结
酮酸饮食对慢性肾病患者的肾功能有保护作用,同时改善患者的营养状况,降低疾病进展速度,值得在临床推广应用。酮酸类似物补充剂增强了LPD的作用,改善了多项指标。当然密切的营养监测和医患沟通也同样重要。
参考文献
[1] Teplan, V., O. Schuck, and O. Mareckova. "Antiproteinuric and metabolic effect of long-term administration ACE inhibitors and angiotensin II AT1 receptor in patients in chronic renal insufficiency." Klin Biochem Metab 11 (2003): 70-73.
[2] Di Iorio, Biagio R., et al. "Phosphate attenuates the anti-proteinuric effect of very low-protein diet in CKD patients." Nephrology Dialysis Transplantation 28.3 (2012): 632-640.
[3] Bellizzi, V., et al. "Very low protein diet supplemented with ketoanalogs improves blood pressure control in chronic kidney disease." Kidney international 71.3 (2007): 245-251.
[4] Brunori, Giuliano, et al. "Efficacy and safety of a very-low-protein diet when postponing dialysis in the elderly: a prospective randomized multicenter controlled study." American Journal of Kidney Diseases 49.5 (2007): 569-580.
[5] Rhee, Connie M., et al. "Low‐protein diet for conservative management of chronic kidney disease: a systematic review and meta‐analysis of controlled trials." Journal of cachexia, sarcopenia and muscle 9.2 (2018): 235-245.
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#CKD患者#
61
#低蛋白饮食#
35
#肾功能#
27
#CRN#
38
#保护作用#
26