JAMA Neurol:原发性进行性失语患者淀粉样蛋白显像研究
2018-01-16 zhangfan MedSci原创
根据现行的分类标准,原发性进行性失语症的诊断与阿尔茨海默生物标志物状态有关,额叶-颞叶变性病理具有高度的预测作用。阿尔茨海默生物标志物阳性可能代表着多种混合病理而非原发性阿尔茨海默病
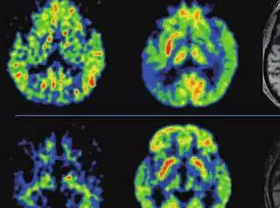
本研究为前瞻性临床病理病例研究,于2002-15年间对患者进行前瞻性纵向评估。PPA的临床诊断方法包括:完整语音、语言和认知测试;认知评估6个月内磁共振成像; PET-C11标记、匹兹堡化合物-B或F18扫描。总计89名PPA患者参与研究,对患者的临床、认知、神经影像学和病理学结果进行分析。
28名患者为影像学支持的语义变体PPA(女性占39.3%,平均年龄64岁),31人为非流畅/无语言变异PPA(女性占71.0%,平均年龄68岁),26人为语言矫正变异PPA(女性占65.4%,平均年龄63岁),4人为混合型PPA。研究发现86%的语义变体以及90%的非流畅/无语言变异PPA患者PET淀粉样病变呈阴性,而96%的语言矫正变异以及75%的混合型PPA患者PET淀粉样病变呈阳性。淀粉样病变阳性的语义变体以及非流畅/无语言变异PPA患者尸检报告发现所有患者均有原发性额颞叶变性和继发性阿尔茨海默病的病理诊断;淀粉样病变阳性的语言矫正变异PPA患者尸检报告确诊患者患有阿尔兹海默症。1名淀粉样病变阴性的混合型PPA患者尸检确证患有皮克病。
根据现行的分类标准,原发性进行性失语症的诊断与阿尔茨海默生物标志物状态有关,额叶-颞叶变性病理具有高度的预测作用。阿尔茨海默生物标志物阳性可能代表着多种混合病理而非原发性阿尔茨海默病。
原始出处:
Miguel A. Santos-Santos et al. Rates of Amyloid Imaging Positivity in Patients With Primary Progressive Aphasia. JAMA Neurol.January 8, 2018.
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#原发性#
32
#进行性#
37
#失语#
47
#Neurol#
42
#淀粉样蛋白#
44