NEJM:非细菌性血栓性心内膜炎-病例报道
2019-06-20 xing.T 网络
与化疗一起,患者开始用低分子量肝素进行抗凝治疗。患者的侧腹疼痛,心内膜炎的外周性表现和心脏瓣膜血栓均已消退。然而,在诊断后7个月,他死于进行性胰腺癌的并发症。
患者为一名健康的48岁男性,因双侧腹疼痛急剧发作而到急诊就诊。在过去的6个月里,他的体重意外减轻了约5公斤。
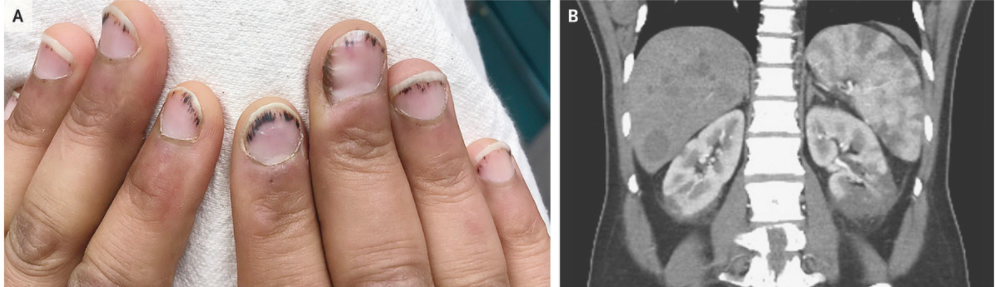
体检时双手指甲上观察到许多碎片状出血(如图A所示)。没有听到心脏杂音,但腹部皮肤很嫩,脾脏在左肋缘下方可触及。抽取血液培养物,并开始针对疑似细菌性心内膜炎进行抗生素治疗。经食道超声心动图显示三尖瓣和二尖瓣上的移位回声灶。腹部的计算机断层扫描显示胰腺颈部肿块,伴有多个肝脏病变,脾脏和肾脏有多个低密度影,这与梗塞一致(如图B所示)。
与化疗一起,患者开始用低分子量肝素进行抗凝治疗。患者的侧腹疼痛,心内膜炎的外周性表现和心脏瓣膜血栓均已消退。然而,在诊断后7个月,他死于进行性胰腺癌的并发症。
原始出处:
John B. Fournier,et al.Nonbacterial Thrombotic Endocarditis.N Engl J Med 2019;https://www.nejm.org/doi/full/10.1056/NEJMicm1804137
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#内膜#
32
#血栓性#
39
#心内膜炎#
27
顶刊就是顶刊,谢谢梅斯带来这么高水平的研究报道,我们科里同事经常看梅斯,分享梅斯上的信息
53
好
65
学习谢谢分享
57