Cell Host Microbe:肠道细菌可变身健康“威胁者”,这竟与自噬有关
2018-02-14 佚名 生物探索
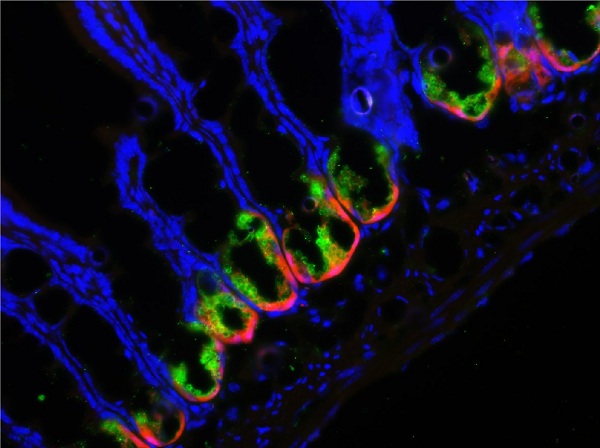
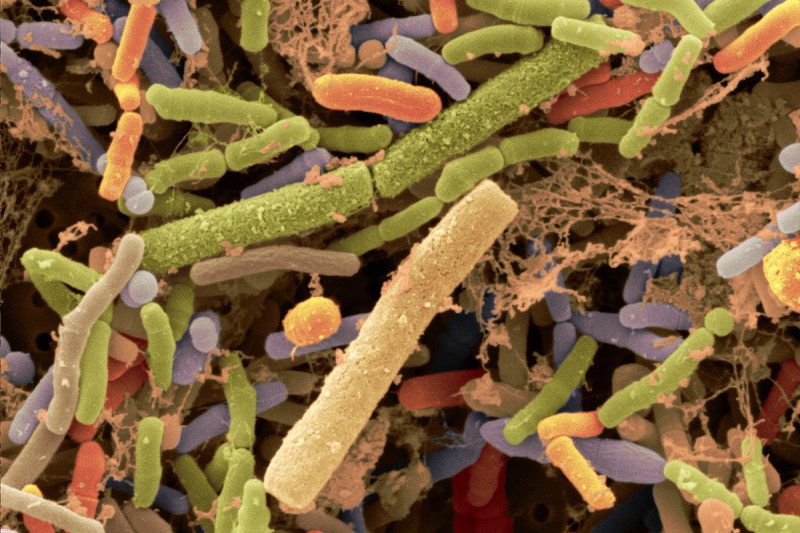
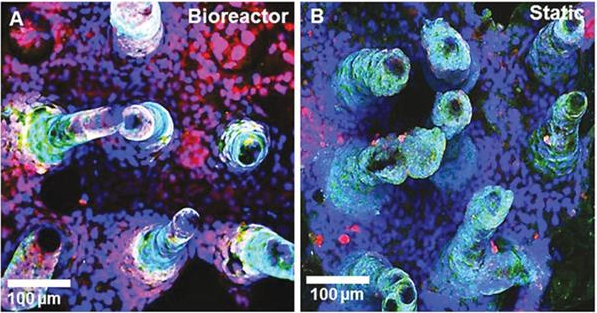
人体微生物——生活在我们体内的数以万亿计的微小细菌——是人类健康重要的参与者。然而,我们与这些生物体的共存机制是非常复杂的。科学家们发现,即使其中出现一点微小变化,也会导致我们的健康出现大问题。

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#Cell#
31
#Micro#
43
#CRO#
29
#CEL#
34
#肠道细菌#
41
学习了.谢谢作者分享!
62
学习了.谢谢作者分享!
64