Kidney int:早发性肾结石的测序研究!
2017-09-14 MedSci MedSci原创
近年来,肾结石的发病率继续上升。此前有研究显示,使用已知可以导致肾结石病的30个基因的基因组测序,可以在11.4%的成人发病的肾结石或肾钙质沉着的个体中以及在16.7-20.8%的18岁以前发病的个体中检测到单因素原因。为了克服测序的局限性,近期,一项发表在杂志Kidney int上的研究在51个家庭中使用了整个外显子测序,这些受试者在25岁以前至少出现一个肾结石或肾脏超声检查发现了肾钙质沉着症,
近年来,肾结石的发病率继续上升。此前有研究显示,使用已知可以导致肾结石病的30个基因的基因组测序,可以在11.4%的成人发病的肾结石或肾钙质沉着的个体中以及在16.7-20.8%的18岁以前发病的个体中检测到单因素原因。
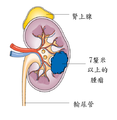
为了克服测序的局限性,近期,一项发表在杂志Kidney int上的研究在51个家庭中使用了整个外显子测序,这些受试者在25岁以前至少出现一个肾结石或肾脏超声检查发现了肾钙质沉着症,此项研究旨在确定潜在的分子遗传病因。
最终,研究者们在51个家庭中的15个,通过整个外显子测序检测到单因因果突变。检测到七个隐性基因(AGXT,ATP6V1B1,CLDN16,CLDN19,GRHPR,SLC3A1,SLC12A1)、一个显性基因(SLC9A3R1)和一个具有隐性和显性遗传的基因(SLC34A1)中出现突变。其中,19种不同突变中的7种以前没有被描述为可致病的。
此项研究建立了整个外显子序列在25岁以前表现为肾结石/肾钙质沉着症的个体中作为分子遗传中的诊断方法。
原始出处:
Daga A, Majmundar AJ, et al. Whole exome sequencing frequently detects a monogenic cause in early onset nephrolithiasis and nephrocalcinosis. Kidney Int. 2017 Sep 8. pii: S0085-2538(17)30494-5. doi: 10.1016/j.kint.2017.06.025.
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#早发#
26
#kidney#
25
学习了.谢谢.
0
学习啦!谢谢分享!
47