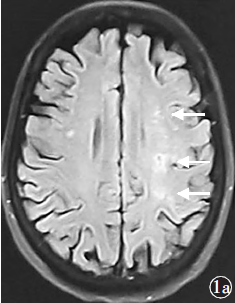
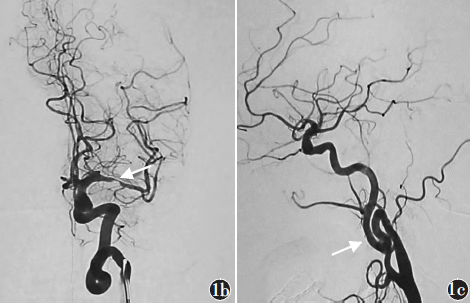
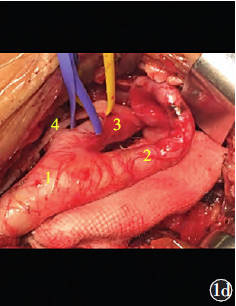
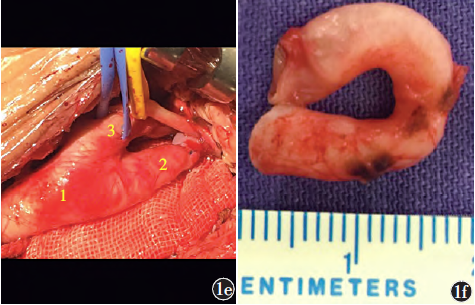
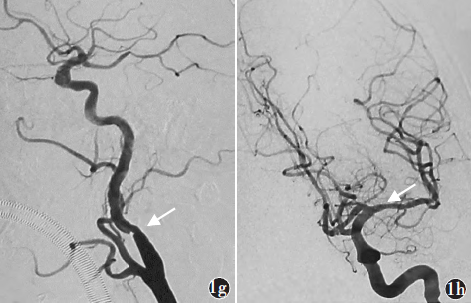
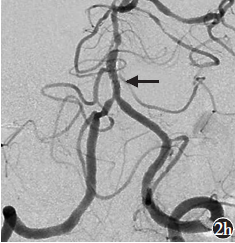
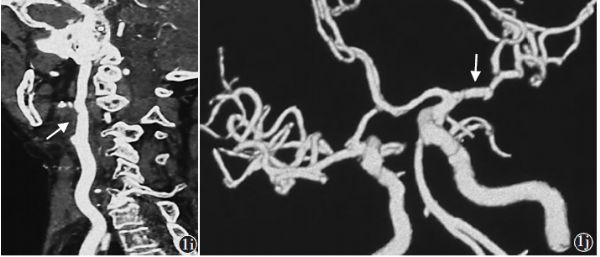
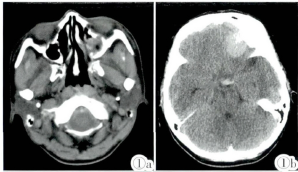
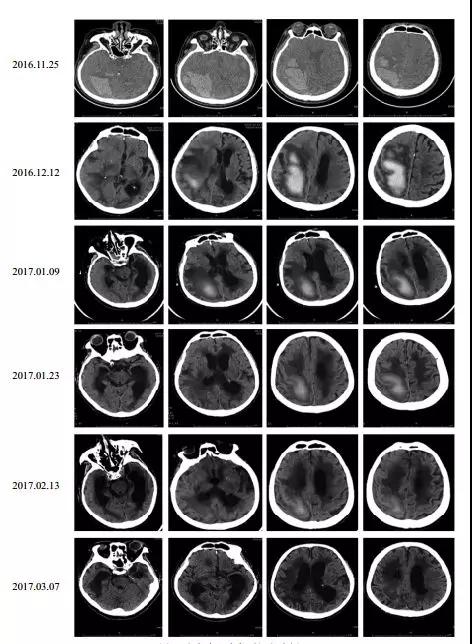
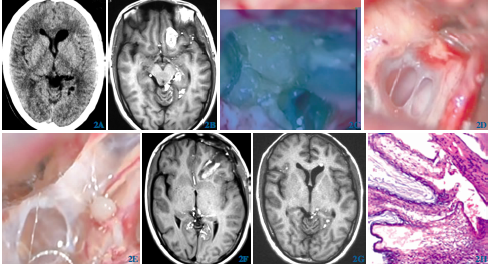
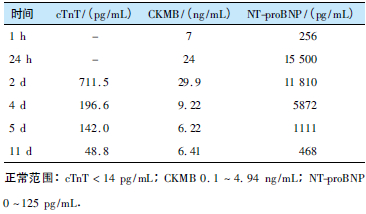
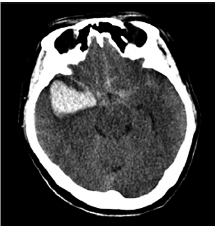
复合手术治疗症状性颅内动脉狭窄合并近端血管迂曲病变二例
2020-01-15 李龙 杨斌 陆夏 中国脑血管病杂志
颅内动脉粥样硬化性狭窄(intracranial atherosclerotic stenosis,ICAS)是导致缺血性卒中的重要原因,尤其好发于亚洲人群。在我国,33%~50%的卒中及50%以上的短暂性脑缺血发作患者存在ICAS。对于经过规范药物治疗仍有症状反复发作的ICAS患者,颅内动脉支架或血管成形术是安全、有效的治疗方式。然而,当ICAS合并近端颈动脉或椎动脉迂曲时,介入治疗的难度和风险
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#颅内动脉狭窄#
35
#近端血管#
29
#手术治疗#
28
#动脉狭窄#
26
#近端#
29