Lancet:左冠状动脉主干疾病治疗之争:CABG优于PCI
2016-11-01 MedSci MedSci原创
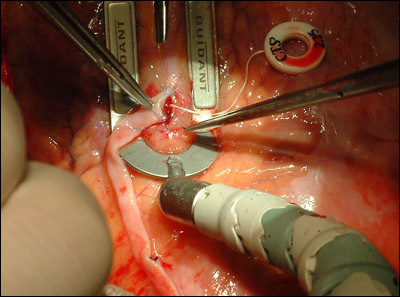
冠状动脉旁路移植术(CABG)是冠状动脉左主干病变患者血运重建的标准治疗方式,不过此方面使用经皮冠状动脉介入治疗(PCI)的适应症也在不断增加。我们的目的是,比较PCI和CABG对左主冠状动脉疾病的治疗效果。在这项前瞻性、随机、开放标签、非劣效性试验中,左主冠状动脉疾病患者来自欧洲北部的36个中心,按1:1随机分到PCI或CABG治疗。符合条件的患者有稳定型心绞痛、不稳定型心绞痛或非ST段抬高型心
冠状动脉旁路移植术(CABG)是左冠状动脉主干病变患者血运重建的标准治疗方式,不过此方面使用经皮冠状动脉介入治疗(PCI)的适应症也在不断增加。我们的目的是,比较PCI和CABG对左冠状动脉主脉疾病的治疗效果(NEJM:左冠状动脉主干疾病治疗之争:这种情况下,PCI不劣于CABG)。
在这项前瞻性、随机、开放标签、非劣效性试验中,左冠状动脉主脉疾病患者来自欧洲北部的36个中心,按1:1随机分到PCI或CABG治疗。符合条件的患者有稳定型心绞痛、不稳定型心绞痛或非ST段抬高型心肌梗死。排除标准为ST段抬高型心肌梗死24小时内,因为这类患者进行CABG或PCI治疗的风险太高,或预期生存期低于1年。
主要研究终点为主要不良心脑血管事件(MACCE),以及全因死亡、非程序性心肌梗死、再次冠状动脉血运重建和卒中发生率。PCI和CABG的非劣效性要求长达5年的随访后,95%可信区间的下端不超过危险比(HR)1.35。
从2008年12月9日到2015年1月21日,纳入1201例患者,PCI组和CABG组分别有598例和603,两组分别有592例患者纳入ITT分析。
PCI组和CABG组的Kaplan Meier 5年MACCE估计分别为29%(121例)和19%(81例),HR 1.48 (95% CI 1.11–1.96),超过了非劣效性的限制,CABG显著优于PCI (p=0·0066)。经治疗的估计分别为28%和19%(1.55, 1.18–2.4, p=0.0015)。PCI组和CABG组的5年估计全因死亡率分别为12%和9%(1.07, 0.67–1.72, p=0.77),非程序性心肌梗死发生率分别为7%和2%(2.88, 1.40–5.90, p=0.0040),血运重建发生率分别为16%和10%(1.50, 1.04–2.17, p=0.032),卒中发病率分别为5%和2%(2.25, 0.93–5.48, p=0.073)。
这项研究的结果表明,左冠状动脉主干疾病的治疗上,CABG优于PCI治疗。
原始出处:
Timo Mäkikallio,et al.Percutaneous coronary angioplasty versus coronary artery bypass grafting in treatment of unprotected left main stenosis (NOBLE): a prospective, randomised, open-label, non-inferiority trial.Lancet.2016.10.30本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#疾病治疗#
25
#Lancet#
25
具体问题具体对待。
63
厲害了~
56
又学习了~
57
学习新知识谢谢。
41
学习一下!
53