JACC&NEJM:有一种卒中和心梗的风险叫带状疱疹?
2017-07-16 麦子 解螺旋·临床医生科研成长平台
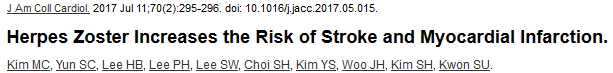
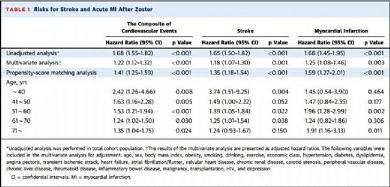
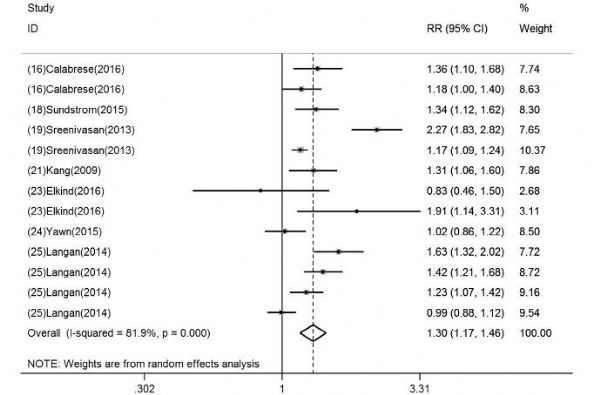
带状疱疹是皮肤科常见病,卒中和心梗则是心脑血管常见病,但二者相加是否还常见呢?似乎报道不是很多。此前国内外都有过散在的病例报道,渐渐也有人注意到它们潜在的联系,做了一些观察性研究。可惜这些研究质量都不太如意,没能提供什么强证据。 但最近一份来自韩国的数据,以Research Letter的形式发在了JACC上,大数据+倾向评分匹配(PSM)分析法,对混杂因素做了控制。Medscape报道了这

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#JACC#
30
#ACC#
24
#疱疹#
25
好文,值得点赞!认真学习,应用于实践!谢谢分享给广大同好!
75
学习了谢谢分享
59
倾向评分匹配法?
64
阅读了谢谢分享
63