Sci Transl Med:聚焦ctDNA长度,提高“滴血验癌”灵敏度!
2019-02-26 M 转化医学网
循环肿瘤DNA(ctDNA)在循环系统的数量往往远远超过血液中非癌症DNA的数量,特别是在肿瘤负荷低的癌症中,或在某些类型的癌症如胶质瘤和肾癌中其数量更是低至难以被准确探测。 改进现有的“滴血验癌”的检测方法对当前利用液体活检发现早期癌症至关重要。
导 读
循环肿瘤DNA(ctDNA)在循环系统的数量往往远远超过血液中非癌症DNA的数量,特别是在肿瘤负荷低的癌症中,或在某些类型的癌症如胶质瘤和肾癌中其数量更是低至难以被准确探测。 改进现有的“滴血验癌”的检测方法对当前利用液体活检发现早期癌症至关重要。 最近由剑桥大学Rosenfeld领导的研究小组领导开发了全新的无细胞肿瘤DNA(cell-free tumor DNA,cftDNA)检测方法,提高了其诊断和治疗癌症的潜力。 在此次研发过程中,研究人员聚焦于ctDNA片段长度,进而提高cftDNA的特异性检测水平。 另一方面,研究人员针对神经胶质瘤患者的脑脊液(CSF)中的cftDNA进行了实验性检测应用。这篇文章发表于最新的《Science Translational Medicine》杂志。
检测90至150bp之间长度的ctDNA或可提高检测灵敏度
在健康个体中,白细胞是cfDNA的主要来源。目前已经开发出基于多种因素预测cfDNA大小的方法,例如利用DNA与组蛋白相互作用进行预测。在某些条件下,例如癌症患者,其他细胞也可以成为ctDNA的来源。片段大小分析增强检测循环肿瘤DNA”。
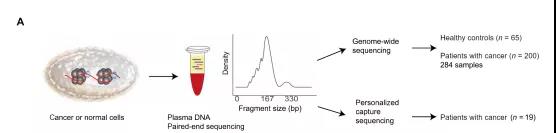
目前改进循环肿瘤DNA(ctDNA)检测水平的方法主要集中于从基因组方向对检测水平进行提高,但很少考虑血浆无细胞DNA(cfDNA)的生物学特性。研究人员假设可以利用循环DNA片段长度的差异来增强检测ctDNA存在的灵敏度和提高癌症的非侵入性基因组分析的水平。Rosenfeld教授使用浅层全基因组测序分析了来自200名癌症患者的344份血浆样本中的ctDNA片段大小。
为了确定突变ctDNA的大小分布,对其中19名患者中进行肿瘤引导的个体化深度测序该团队检测到肿瘤相关片段在90至150bp之间长度的ctDNA富集,具地说,研究人员在患有黑素瘤,乳腺癌,卵巢癌,肺癌,结肠直肠癌和胆管癌癌症的患者中发现20至150bp的肿瘤相关ctDNA片段,但在其他癌症的血浆样品中并没有发现类似长度的ctDNA。
在明确肿瘤类型与短序列ctDNA之间的关联性后,研究人员基于此开发了对这些小片段进行体外检测和相应的计算机辅助筛选方法。通过机器学习模型分析和利用cfDNA的全基因组碎片,采用简单便宜的测序方法,研究人员可以大大提高检测血液循环中微量肿瘤衍生分子的灵敏度。
他们在没有预先明确患者突变或拷贝数改变的情况下完成了这项测试工作。利用90至150 bp之间的ctDNA片段大大提高了肿瘤DNA的检测对平,其在> 95%的病例中中值富集超过两倍,在> 10%的病例中富集数超过四倍。
奥地利格拉茨医科大学分子生物遗传研究中心的Ellen Heitzer博士和Michael Speicher医学博士评论道,“该研究大大提高了基于cfDNA的诊断测试的安全性。对患有早期癌症的患者进行安全、有效的诊断鉴别一方面可提高患者的治疗预后,另一方面可大大降低患者进行癌前诊断的成本”。
ctDNA检测在脑肿瘤的应用
同样还是Rosenfeld的团队,他们在循环血液中测试并开发提高ctDNA的方法后,又将目光投向了脑脊液。该团队的研究成员探讨了改进现有用于脑部肿瘤液体活检的方法。其最新的成果发表于最新的《EMBO》
由于脑胶质瘤患者血浆中cftDNA的检出率极低,因此脑脊液(CSF)检测一直是一种诱人的替代方法。然而,CSF中cftDNA的检测存在许多挑战,并且取决于肿瘤的位置和异质性。
使用当前的液体活组织检查方法难以检测或表征胶质瘤。 先前提出检测脑脊液(CSF)中的无细胞肿瘤DNA(cftDNA)作为血浆检测的替代方案。 此次Rosenfeld的团队使用浅层全基因组测序(sWGS)对13名原发性胶质瘤患者的CSF的无细胞DNA进行测序进而明确体细胞拷贝数改变和DNA片段化模式。
这使研究人员能够明确CSF中的cftDNA,而事先明确肿瘤中存在的点突变。同时研究人员还发现CSF中无细胞DNA的碎裂模式与血浆中的碎裂模式并不相同。 这种低成本的筛选方法可提供有关肿瘤基因组的信息,可用于针对具有高水平cftDNA的患者进行进一步的大规模测序。
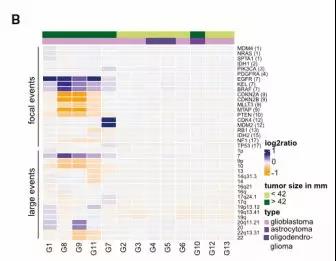
Rosenfeld教授指出,SCNA和sWGS的组合对cfDNA的片段化分析提供了一种快速,低成本的筛选方法,其可提供肿瘤基因组信息。反过来,这可以针对具有高水平cftDNA的患者进行更大规模的全外显子组或全基因组测序。并且,将液体活检的应用潜力扩展到更多患有不同类型癌症的患者当中去,进而大大改善目前液体活检的现状。
原始出处:Mouliere F, Chandrananda D, Piskorz AM, et al. Enhanced detection of circulating tumor DNA by fragment size analysis. Sci Transl Med. 2018 Nov 7;10(466).
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言






#TRA#
32
#滴血验癌#
38
#灵敏度#
54
提高CtDNA的敏感度,同时确定测序的基因对诊断和随访价值重大
72
#Transl#
35
好
64
#Med#
25
谢谢了,学习
57