Adv Healthc Mater:3D生物打印有望实现复杂空腔组织或器官的精准构建 仁济医院与哈佛医学院联合发表研究成果
2018-11-16 佚名 科学网
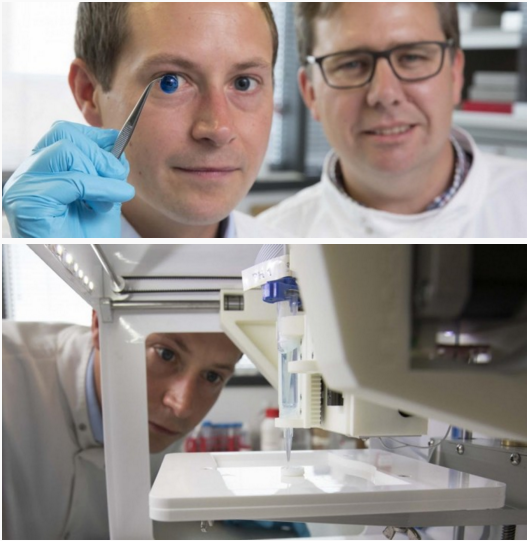
将各种功能细胞注入打印机精准构建复层空腔组织,这是科学创意还是现实?近日,上海交通大学医学院附属仁济医院整形外科皮庆猛博士在国际生物材料顶级杂志Advanced Materials(最新影响因子21.95)在线发表题为“多层环状组织的数字可调微流控生物打印”(Digitally Tunable Microflidic Bioprinting of Multilayered Cannular Tis
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#研究成果#
26
#3D生物打印#
40
#ALT#
26
#医学院#
28
这个确实是前沿
53
#3D#
26
#精准#
32
#仁济医院#
34
#哈佛医学院#
36
#哈佛#
21