cell:免疫细胞的衰老,主因是环境:Cell揭示根源
2018-04-28 Flora 生物探索
为什么年纪大了,免疫力会下降?为什么免疫系统的衰老速度会因人而异?为什么相比于遗传,环境对于免疫系统的影响程度更大?近期,科学家们通过分析单个细胞内染色质的差异,找到了回答这些问题的新线索。
来自于斯坦福大学医学院的科学家们完成了这一庞大的工作,分析了大量免疫细胞。他们发现,相比于年轻人,老年人的免疫细胞携带更多的染色质修饰。而且,这些修饰差异主要来源于环境。
研究团队的关注点在于组蛋白(与细胞核内DNA紧密结合的蛋白结构)修饰,是表观遗传学的重要部分,后者在健康、疾病领域有着不容忽视的地位。相关研究成果在线发表在最新一期的《Cell》上。doi.org/10.1016/j.cell.2018.03.079
1表观遗传学的影响
蛋白质是执行细胞活动的主力。一个细胞的身份、功能与其表达的蛋白质类型、数量密切相关。事实上,体内的每一个细胞都含有相同的DNA,但是皮肤细胞、脂肪细胞和神经细胞表达的蛋白质却有着很大的差异,因此,它们各自执行的功能不同。通过指定基因表达与否,DNA序列上的表观遗传标记很大程度上指引、定义了细胞的整体行为。
“除去变异或者染色体末端磨损,DNA在衰老的过程中基本保持不变,但是基因的表达程度却可能经历着大的变化。”文章通讯作者免疫学和风湿病学教授Paul J. Utz表示道。
此外,伴随着细胞的分裂、衰老等过程,表观遗传修饰会不断变化。其中,免疫系统中大量白细胞的基因表达水平会伴随着衰老而发生显着的变化。
考虑到这些,研究团队推测,免疫细胞发生与衰老相关的变化,可能源于组蛋白修饰的变化。他们想知道,不同免疫细胞类型受表观遗传标记变化影响的程度,而且这种影响模式在不同人之间或者同一个个体不同细胞的差异。
2衰老的免疫细胞
Paul J. Utz和生物信息学助理教授Purvesh Khatri、基础生命科学研究副研究员Alex Kuo和博士后Francesco Vallania合作,利用质谱流式细胞技术(mass cytometry)从单细胞水平分析了免疫细胞的染色质修饰情况。他们分析了22种不同免疫细胞内40种不同类型的表观遗传标记,共积累了约217亿个数据点,并进行了专门的数据解析。
结果发现,许多衰老的免疫细胞比年轻的免疫细胞携带更多的组蛋白标记。此外,相比于年轻人,老年人免疫细胞之间的组蛋白修饰差异性更大。
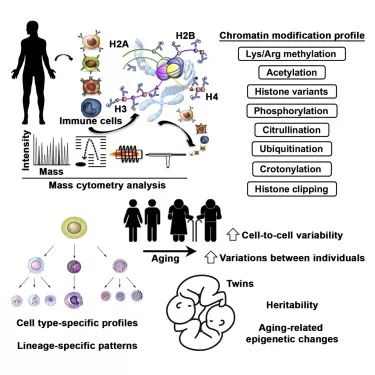
3变化主要源于环境
为了评估环境、遗传对于组蛋白标记模式的影响差异,研究人员从同卵双胞胎、异卵双胞胎中获取血液样本。其中,同卵双胞胎拥有相同的DNA序列,分享着共同的宫内环境。虽然异卵双胞胎DNA有差异,但是宫内环境、成长环境(一起长大)相同。
结果显示,相比于年轻的同卵双胞胎,年老的同卵双胞胎之间的组蛋白修饰差异较大。而且这些差异相当于两个完全没有血缘关系的人。进一步数据分析表明,老年人表现出的表观遗传差异主要源于非遗传因素,包括饮食、睡眠、运动、感染、工作、居住的地方,以及生理、心理压力等。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#Cell#
32
#CEL#
29
学习了.长知识
56
谢谢分享学习
60
学习了.谢谢分享
50