Eur Respir J:非流感病毒所致成人社区获得性肺炎病情严重程度与预后——一项来自CAP-China中国肺炎研究网的前瞻性注册登记研究
2019-06-23 周飞 呼吸界
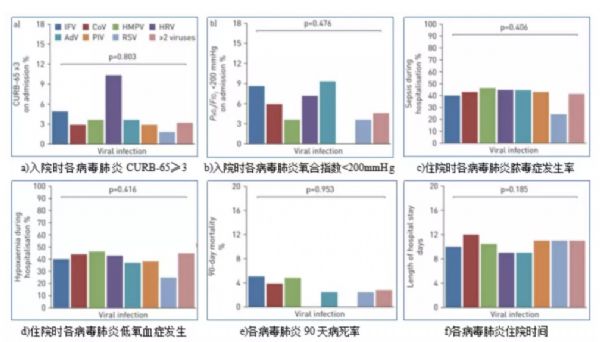
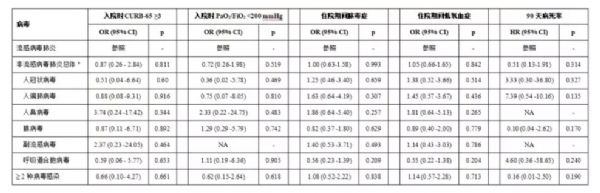
本研究比较了非免疫抑制成人流感与非流感病毒所致 CAP 的病情严重程度、达临床稳定时间、并发症、病死率及住院时间等,首次系统性评估了成人非流感病毒肺炎的临床意义,研究论文 2019 年 6 月 4 日在欧洲呼吸杂志在线发表。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#前瞻性#
25
#CHINA#
41
#CAP#
45
#获得性#
39
#病情#
33
#社区#
23
#注册#
34
学习了
62