Cell:效果喜人!多国科学家首次证明,溶瘤病毒联合PD-1抑制剂免疫治疗可以大幅提升癌症响应率
2017-09-25 刘盼盼 王新凯 奇点网
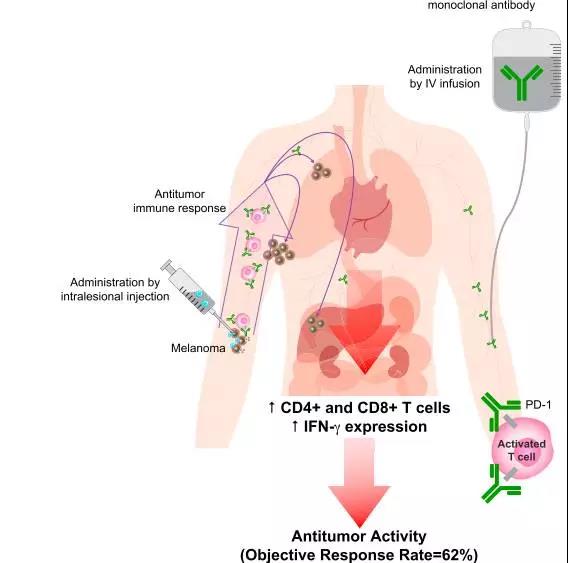
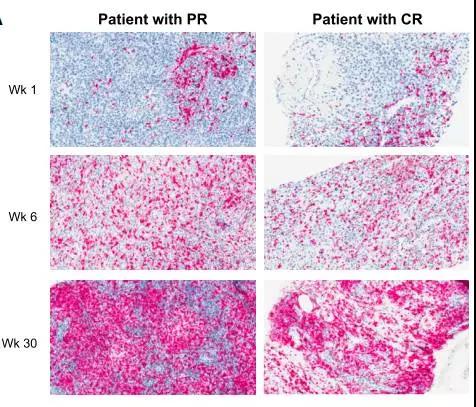
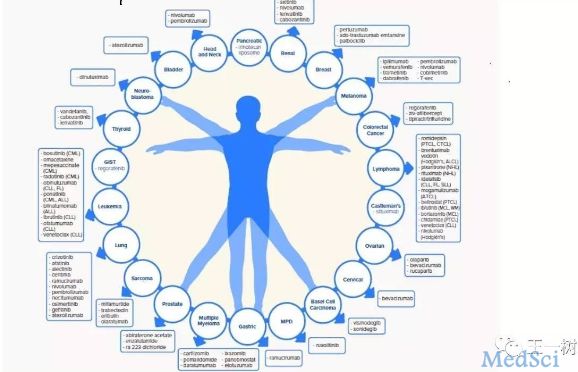
研究人员先是向黑色素瘤局部注射溶瘤病毒,破坏肿瘤微环境,然后全身系统性静脉应用PD-1抑制剂,激活和增强T细胞对肿瘤细胞的攻击和杀伤。这就好比围剿敌方老巢时,先发射导弹进行战略轰炸,再派特种部队全面清剿。

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#抑制剂#
27
#CEL#
30
#Cell#
33
#PD-1抑制剂#
32
学习了谢谢作者分享!
79
谢谢分享.学习
87