JAHA:NT‐proBNP在成年先心病患者中的预后价值
2018-04-04 MedSci MedSci原创
N末端B型利钠肽(NT‐proBNP)是成年先心病患者预后的可靠预测指标。本研究的目的旨在评估 NT‐proBNP在成年先心病患者中的水平以及其与心血管不良事件发生的相关性。本研究纳入了2011年至2013年门诊诊断的602名成年先心病患者,其中对595名(平均年龄为33岁,男性占58%,90%患者的纽约心功能分级为I级)患者的 NT‐proBNP水平进行了检测,并每年进行了随访,主要终点事件是死
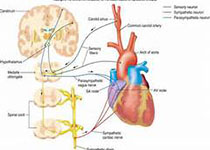
N末端B型利钠肽(NT‐proBNP)是成年先心病患者预后的可靠预测指标。本研究的目的旨在评估 NT‐proBNP在成年先心病患者中的水平以及其与心血管不良事件发生的相关性。本研究纳入了2011年至2013年门诊诊断的602名成年先心病患者,其中对595名(平均年龄为33岁,男性占58%,90%患者的纽约心功能分级为I级)患者的 NT‐proBNP水平进行了检测,并每年进行了随访,主要终点事件是死亡、心衰、住院、心律失常血栓栓塞事件和心脏介入干预。经过平均4.4年时间的随访,共有199名患者出现主要终点事件,主要终点事件前一年的NT‐proBNP水平平均升高2.9 pmol/L,次要终点事件升高了18.2 pmol/L,而没有出现终点事件患者的仅升高了0.3 pmol/L(p<0.001)。研究结果显示,成年先心病患者在出现心血管不良事件之前的NT‐proBNP水平是明显升高的,尤其是死亡和心衰。原始出处:Vivan J et al.Prognostic Value of Serial N‐Terminal Pro‐B‐Type Natriuretic Peptide Measurem
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#AHA#
33
#BNP#
30
#先心病#
39
#预后价值#
34
#PRO#
40