Lancet:卡培他滨联合贝伐单抗治疗转移性结肠癌效果良好
2015-04-08 姜英浩译 MedSci原创
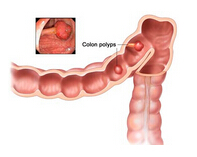
目前,在临床上针对转移性结肠癌的一线治疗方式:化疗联合北伐单抗疗法的最优治疗时间仍然是未知的。CAIRO3试验的研究目的在于评估卡培他滨联合贝伐单抗进行维持治疗与观察组相比疗效何如。该结果在线发表于2015年4月8日的The Lancet杂志上。 该研究是一项开放、随机对照的3期临床试验。研究人员从荷兰国内64个医院招募受试患者。纳入标准为年龄大于18岁,患转移性结肠癌,未曾接受过治疗,在6个3
目前,在临床上针对转移性结肠癌的一线治疗方式:化疗联合北伐单抗疗法的最优治疗时间仍然是未知的。CAIRO3试验的研究目的在于评估卡培他滨联合贝伐单抗进行维持治疗与观察组相比疗效何如。该结果在线发表于2015年4月8日的The Lancet杂志上。
该研究是一项开放、随机对照的3期临床试验。研究人员从荷兰国内64个医院招募受试患者。纳入标准为年龄大于18岁,患转移性结肠癌,未曾接受过治疗,在6个3周为周期的卡培他滨/奥沙利铂/贝伐单抗(CAPOX-B)的诱导治疗后疾病状态稳定或较好,WHO评分0-1,骨髓、肝脏、肾脏功能正常。将所有受试患者按1:1比例随机分配至观察组或维持组,维持组给予卡培他滨和贝伐单抗治疗。通过中央最小化进行随机化分组,根据既往辅助性化疗、对诱导治疗的应答水平、WHO评分、血清乳酸脱氢酶含量、治疗中心等进行分层。所有受试者与研究者对分组情况均知晓。每9周评估一次疾病状态。疾病第一次进展时(PFS1),患者均接受CAPOX-B诱导治疗直至第二次进展(PFS2),主要评估指标为第二次疾病进展。所有终点事件均从随机化开始时进行计算。通过意向治疗进行分析。
结果显示,从2007年5月30日至2012年10月15日,共有558名患者参与了随机分组,维持组与观察组各279例。中位随访期为48个月(IQR36-57)。维持组的主要评估指标——中位PFS2较观察组有显著提升:观察组8.5个月,维持组11.7个月(HR 0•67, 95% CI 0•56–0•81, p<0•0001)。当PFS1发生后进行任何治疗,该差异仍保持显著。维持组的药物耐受性更好,尽管该组手-足综合征发病率有所增加(在维持治疗过程中64例[23 %]患者出现手-足皮肤反应)。在维持治疗中,整体生存质量未出现恶化现象,两组临床指标未有明显不同。
因此作者得出结论:在治疗转移性结肠癌患者时,在6个周期的CAPOX-B治疗后给予卡培他滨联合贝伐单抗进行维持治疗能够有效控制疾病并且不会影响生活质量。
临床注册号:ClinicalTrials.gov, number NCT00442637。
原文出处:
Lieke H J Simkens, Harm van Tinteren, Anne May, et al. Maintenance treatment with capecitabine and bevacizumab in metastatic colorectal cancer (CAIRO3): a phase 3 randomised controlled trial of the Dutch Colorectal Cancer Group. The Lancet. 2015.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












北伐单抗?
26
#Lancet#
37
#卡培他滨#
36
#转移性#
32
#贝伐#
34
谢谢了
123